A teratoma is a tumor made up of several different types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the tailbone, ovary, or testicle.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.

A dermoid cyst is a teratoma of a cystic nature that contains an array of developmentally mature, solid tissues. It frequently consists of skin, hair follicles, and sweat glands, while other commonly found components include clumps of long hair, pockets of sebum, blood, fat, bone, nail, teeth, eyes, cartilage, and thyroid tissue.

Pseudomyxoma peritonei (PMP) is a clinical condition caused by cancerous cells that produce abundant mucin or gelatinous ascites. The tumors cause fibrosis of tissues and impede digestion or organ function, and if left untreated, the tumors and mucin they produce will fill the abdominal cavity. This will result in compression of organs and will destroy the function of the colon, small intestine, stomach, or other organs. Prognosis with treatment in many cases is optimistic, but the disease is lethal if untreated, with death occurring via cachexia, bowel obstruction, or other types of complications.

A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

Pseudocysts are like cysts, but lack epithelial or endothelial cells. Initial management consists of general supportive care. Symptoms and complications caused by pseudocysts require surgery. Computed tomography (CT) scans are used for initial imaging of cysts, and endoscopic ultrasounds are used in differentiating between cysts and pseudocysts. Endoscopic drainage is a popular and effective method of treating pseudocysts.
Pancreatic diseases are diseases that affect the pancreas, an organ in most vertebrates and in humans and other mammals located in the abdomen. The pancreas plays a role in the digestive and endocrine system, producing enzymes which aid the digestion process and the hormone insulin, which regulates blood sugar levels. The most common pancreatic disease is pancreatitis, an inflammation of the pancreas which could come in acute or chronic form. Other pancreatic diseases include diabetes mellitus, exocrine pancreatic insufficiency, cystic fibrosis, pseudocysts, cysts, congenital malformations, tumors including pancreatic cancer, and hemosuccus pancreaticus.

A dentigerous cyst, also known as a follicular cyst, is an epithelial-lined developmental cyst formed by accumulation of fluid between the reduced enamel epithelium and the crown of an unerupted tooth. It is formed when there is an alteration in the reduced enamel epithelium and encloses the crown of an unerupted tooth at the cemento-enamel junction. Fluid is accumulated between reduced enamel epithelium and the crown of an unerupted tooth.

An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life. Odontogenic keratocysts make up around 19% of jaw cysts.

Calcifying odontogenic cyst (COC) is a rare developmental lesion that comes from odontogenic epithelium. It is also known as a calcifying cystic odontogenic tumor, which is a proliferation of odontogenic epithelium and scattered nest of ghost cells and calcifications that may form the lining of a cyst, or present as a solid mass.

A persistent thyroglossal duct is a usually benign medical condition in which the thyroglossal duct, a structure usually only found during embryonic development, fails to atrophy. The duct persists as a midline structure forming an open connection between the back of the tongue and the thyroid gland. This opening can lead to fluid accumulation and infection, which necessitate the removal of the duct.
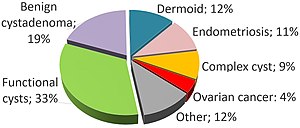
Ovarian diseases refer to diseases or disorders of the ovary.
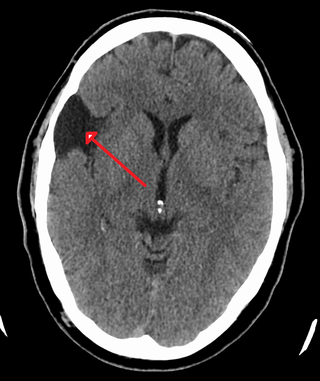
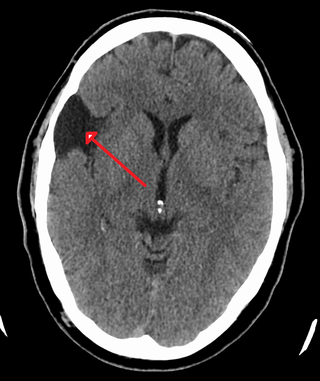
A central nervous system cyst is a type of cyst that presents and affects part of the central nervous system (CNS). They are usually benign and filled with either cerebrospinal fluid, blood, or tumor cells. CNS cysts are classified into two categories: cysts that originate from non-central nervous system tissue, migrate to, and form on a portion of the CNS, and cysts that originate within central nervous system tissue itself. Within these two categories, there are many types of CNS cysts that have been identified from previous studies.
Vanishing bile duct syndrome is a loose collection of diseases which leads to the injury to hepatic bile ducts and eventual ductopenia.
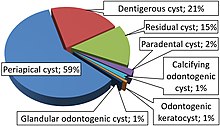
Odontogenic cyst are a group of jaw cysts that are formed from tissues involved in odontogenesis. Odontogenic cysts are closed sacs, and have a distinct membrane derived from rests of odontogenic epithelium. It may contain air, fluids, or semi-solid material. Intra-bony cysts are most common in the jaws, because the mandible and maxilla are the only bones with epithelial components. That odontogenic epithelium is critical in normal tooth development. However, epithelial rests may be the origin for the cyst lining later. Not all oral cysts are odontogenic cysts. For example, mucous cyst of the oral mucosa and nasolabial duct cyst are not of odontogenic origin.

An endolymphatic sac tumor (ELST) is a very uncommon papillary epithelial neoplasm arising within the endolymphatic sac or endolymphatic duct. This tumor shows a very high association with Von Hippel–Lindau syndrome (VHL).

A Gartner's duct cyst is a benign vaginal cyst that originates from the Gartner's duct, which is a vestigial remnant of the mesonephric duct in females. Persistent Wolffian duct syndrome (PWDS) in individuals with XX chromosomes is the inverse disorder of Persistent Müllerian duct syndrome (PMDS) in individuals with XY chromosomes. They are typically small asymptomatic cysts that occur along the lateral walls of the vagina, following the course of the duct. They can present in adolescence with painful menstruation (dysmenorrhea) or difficulty inserting a tampon. They can also enlarge to substantial proportions and be mistaken for urethral diverticulum or cystocele. In some rare instances, they can be congenital.

Vaginal cysts are uncommon benign cysts that develop in the vaginal wall. The type of epithelial tissue lining a cyst is used to classify these growths. They can be congenital. They can present in childhood and adulthood. The most common type is the squamous inclusion cyst. It develops within vaginal tissue present at the site of an episiotomy or other vaginal surgical sites. In most instances they do not cause symptoms and present with few or no complications. A vaginal cyst can develop on the surface of the vaginal epithelium or in deeper layers. Often, they are found by the woman herself and as an incidental finding during a routine pelvic examination. Vaginal cysts can mimic other structures that protrude from the vagina such as a rectocele and cystocele. Some cysts can be distinguished visually but most will need a biopsy to determine the type. Vaginal cysts can vary in size and can grow as large as 7 cm. Other cysts can be present on the vaginal wall though mostly these can be differentiated. Vaginal cysts can often be palpated (felt) by a clinician. Vaginal cysts are one type of vaginal mass, others include cancers and tumors. The prevalence of vaginal cysts is uncertain since many go unreported but it is estimated that 1 out of 200 women have a vaginal cyst. Vaginal cysts may initially be discovered during pregnancy and childbirth. These are then treated to provide an unobstructed delivery of the infant. Growths that originate from the urethra and other tissue can present as cysts of the vagina.
Vulvar tumors are those neoplasms of the vulva. Vulvar and vaginal neoplasms make up a small percentage (3%) of female genital cancers. They can be benign or malignant. Vulvar neoplasms are divided into cystic or solid lesions and other mixed types. Vulvar cancers are those malignant neoplasms that originate from vulvar epithelium, while vulvar sarcomas develop from non-epithelial cells such as bone, cartilage, fat, muscle, blood vessels, or other connective or supportive tissue. Epithelial and mesenchymal tissue are the origin of vulvar tumors.