Campylobacter is a genus of Gram-negative bacteria. Campylobacter typically appear comma- or s-shaped, and are motile.
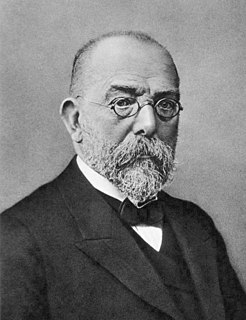
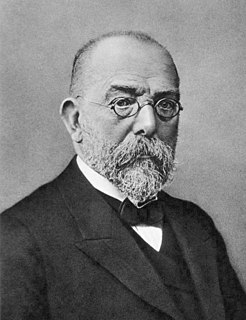
Koch's postulates are four criteria designed to establish a causative relationship between a microbe and a disease. The postulates were formulated by Robert Koch and Friedrich Loeffler in 1884, based on earlier concepts described by Jakob Henle, and refined and published by Koch in 1890. Koch applied the postulates to describe the etiology of cholera and tuberculosis, but they have been controversially generalized to other diseases. These postulates were generated before modern concepts in microbial pathogenesis that cannot be examined using Koch's postulates, including viruses and asymptomatic carriers. They have largely been supplanted by other criteria such as the Bradford Hill criteria for infectious disease causality in modern public health.

Helicobacter pylori, previously known as Campylobacter pylori, is a gram-negative, helically-shaped, microaerophilic bacterium usually found in the stomach. Its helical shape is thought to have evolved in order to penetrate the mucoid lining of the stomach and thereby establish infection. The bacterium was first identified in 1982 by Australian doctors Barry Marshall and Robin Warren. H. pylori has been associated with the mucosa-associated lymphoid tissue in the stomach, esophagus, colon, rectum, or tissues around the eye, and of lymphoid tissue in the stomach.

Helicobacter is a genus of Gram-negative bacteria possessing a characteristic helical shape. They were initially considered to be members of the genus Campylobacter, but in 1989, Goodwin et al. published sufficient reasons to justify the new genus name Helicobacter. The genus Helicobacter contains about 35 species.
Virulence is a pathogen's or microbe's ability to infect or damage a host.

Giardiasis, popularly known as beaver fever, is a parasitic disease caused by Giardia duodenalis. About 10% of those infected have no symptoms. When symptoms occur they may include diarrhea, abdominal pain, and weight loss. Vomiting, blood in the stool, and fever are less common. Symptoms usually begin 1 to 3 weeks after exposure and without treatment may last up to six weeks.

Gastritis is inflammation of the lining of the stomach. It may occur as a short episode or may be of a long duration. There may be no symptoms but, when symptoms are present, the most common is upper abdominal pain. Other possible symptoms include nausea and vomiting, bloating, loss of appetite and heartburn. Complications may include stomach bleeding, stomach ulcers, and stomach tumors. When due to autoimmune problems, low red blood cells due to not enough vitamin B12 may occur, a condition known as pernicious anemia.

Travelers' diarrhea (TD) is a stomach and intestinal infection. TD is defined as the passage of unformed stool while traveling. It may be accompanied by abdominal cramps, nausea, fever, and bloating. Occasionally bloody diarrhea may occur. Most travelers recover within four days with little or no treatment. About 10% of people may have symptoms for a week.
Dientamoebiasis is a medical condition caused by infection with Dientamoeba fragilis, a single-cell parasite that infects the lower gastrointestinal tract of humans. It is an important cause of traveler's diarrhea, chronic abdominal pain, chronic fatigue, and failure to thrive in children.

This is a timeline of the events relating to the discovery that peptic ulcer disease and some cancers are caused by H. pylori. In 2005, Barry Marshall and Robin Warren were awarded the Nobel Prize in Physiology or Medicine for their discovery that peptic ulcer disease (PUD) was primarily caused by Helicobacter pylori, a bacterium with affinity for acidic environments, such as the stomach. As a result, PUD that is associated with H. pylori is currently treated with antibiotics used to eradicate the infection. For decades prior to their discovery, it was widely believed that PUD was caused by excess acid in the stomach. During this time, acid control was the primary method of treatment for PUD, to only partial success. Among other effects, it is now known that acid suppression alters the stomach milieu to make it less amenable to H. pylori infection.
Saccharomyces boulardii is a tropical species of yeast first isolated from lychee and mangosteen fruit in 1923 by French scientist Henri Boulard. Although early reports described distinct taxonomic, metabolic, and genetic properties, S. boulardii is a strain of S. cerevisiae, sharing >99% genomic relatedness, giving the synonym S. cerevisiae var boulardii. A type strain is Hansen CBS 5926.

Blastocystis is a genus of single-celled heterokont parasites belonging to a group of organisms that are known as the Stramenopiles that includes algae, diatoms, and water molds. Blastocystis consists of several species, living in the gastrointestinal tracts of species as diverse as humans, farm animals, birds, rodents, reptiles, amphibians, fish, and cockroaches. Blastocystis exhibits low host specificity, and many different species of Blastocystis can infect humans, and by current convention, any of these species would be identified as Blastocystis hominis.

Blastocystosis refers to a medical condition caused by infection with Blastocystis. Blastocystis is a protozoal, single-celled parasite that inhabits the gastrointestinal tracts of humans and other animals. Many different types of Blastocystis exist, and they can infect humans, farm animals, birds, rodents, amphibians, reptiles, fish, and even cockroaches. Blastocystosis has been found to be a possible risk factor for development of irritable bowel syndrome.
In biology, a pathogen in the oldest and broadest sense, is any organism that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ.
The host–pathogen interaction is defined as how microbes or viruses sustain themselves within host organisms on a molecular, cellular, organismal or population level. This term is most commonly used to refer to disease-causing microorganisms although they may not cause illness in all hosts. Because of this, the definition has been expanded to how known pathogens survive within their host, whether they cause disease or not.
Helicobacter felis is a bacterium species in the Helicobacteraceae family, Campylobacterales order, Helicobacter genus. This bacterium is Gram-negative, microaerophilic, urease-positive, and spiral-shaped. Its type strain is CS1T. It can be pathogenic.
Helicobacter salomonis is a species within the Helicobacter genus of Gram negative bacteria. Helicobacter pylori is by far the best known Helicobacter species primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, doudenal ulcers, stomach cancers of the non-lymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study. Humans infected with H. salomonis may develop some of the same gastrointestinal diseases viz., stomach inflammation, stomach ulcers, duodenum ulcers, stomach cancers that are not lymphomas, and extrnodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter bizzozeronii, Helicobacter suis, Helicobacter felis, and Helicobacter heilmannii s.s Because of their disease associations, these four Helicobacter species plus H. salomonis are often group together and termed Helicobacter heilmannii sensu lato.
Helicobacter bizzozeronii is a species within the Helicobacter genus of Gram negative bacteria. Helicobacter pylori is by far the best known Helicobacter species primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, doudenal ulcers, stomach cancers of the non-lymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study. Humans infected with H. bizzozeronii are prone to develop some of the same gastrointestinal diseases viz., stomach inflammation, stomach ulcers, duodenum ulcers, stomach cancers that are not lymphomas, and extrnodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter felis, Helicobacter salomonis, Helicobacter suis, and Helicobacter heilmannii s.s. Because of their disease associations, these four Helicobacter species plus H. bizzozeronii are often group together and termed Helicobacter heilmannii sensu lato.
Helicobacter suis is a species within the Helicobacter genus of Gram negative bacteria. Helicobacter pylori is by far the best known Helicobacter species primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, doudenal ulcers, stomach cancers of the non-lymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study. Humans infected with H. suis may develop some of the same gastrointestinal diseases viz., stomach inflammation, stomach ulcers, duodenum ulcers, stomach cancers that are not lymphomas, and extrnodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter bizzozeronii, Helicobacter salomonis, Helicobacter felis, and Helicobacter heilmannii s.s. Because of their disease associations, these four Helicobacter species plus H. suis are often group together and termed Helicobacter heilmannii sensu lato.
Helicobacter heilmannii s.s. is a species within the Helicobacter genus of Gram negative bacteria. Helicobacter pylori is by far the best known Helicobacter species primarily because humans infected with it may develop gastrointestinal tract diseases such as stomach inflammation, stomach ulcers, doudenal ulcers, stomach cancers of the non-lymphoma type, and various subtypes of extranodal marginal zone lymphomass, e.g. those of the stomach, small intestines, large intestines, and rectumn. H. pylori is also associated with the development of bile duct cancer and has been associated with a wide range of other diseases although its role in the development of many of these other diseases requires further study. Humans infected with H. heilmannii s.s. may develop some of the same gastrointestinal diseases viz., stomach inflammation, stomach ulcers, duodenum ulcers, stomach cancers that are not lymphomas, and extranodal marginal B cell lymphomas of the stomach. Other non-H. pylori Helicobacter species that are known to be associated with these gastrointestinal diseases are Helicobacter bizzozeronii, Helicobacter suis, Helicobacter felis, and Helicobacter salomonis. Because of their disease associations, these four Helicobacter species plus H. heilmannii s.s. are often group together and termed Helicobacter heilmannii sensu lato.