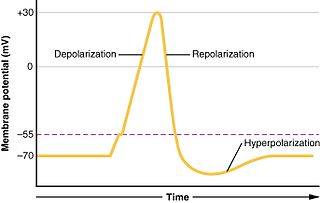
Electrocardiography is the process of producing an electrocardiogram, a recording - a graph of voltage versus time - of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances, inadequate coronary artery blood flow, and electrolyte disturbances.

The systole is the part of the cardiac cycle during which some chambers of the heart muscle contract after refilling with blood. The term "systole" originates from New Latin via Ancient Greek συστολή (sustolē): from συστέλλειν via [σύν + στέλλειν. The use of systole, "to contract", is very similar to the use of the English term "to squeeze".
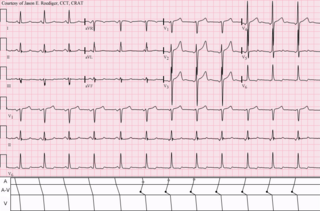
Wolff–Parkinson–White syndrome (WPWS) is a disorder due to a specific type of problem with the electrical system of the heart which has resulted in symptoms. About 40% of people with the electrical problem never develop symptoms. Symptoms can include an abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, or syncope. Rarely, cardiac arrest may occur. The most common type of irregular heartbeat that occurs is known as paroxysmal supraventricular tachycardia.

The ostium primum atrial septal defect is a defect in the atrial septum at the level of the tricuspid and mitral valves. This is sometimes known as an endocardial cushion defect because it often involves the endocardial cushion, which is the portion of the heart where the atrial septum meets the ventricular septum and the mitral valve meets the tricuspid valve.

The jugular venous pressure is the indirectly observed pressure over the venous system via visualization of the internal jugular vein. It can be useful in the differentiation of different forms of heart and lung disease. Classically three upward deflections and two downward deflections have been described.

Supraventricular tachycardia (SVT) is an abnormally fast heart rhythm arising from improper electrical activity in the upper part of the heart. There are four main types: atrial fibrillation, paroxysmal supraventricular tachycardia (PSVT), atrial flutter, and Wolff–Parkinson–White syndrome. Symptoms may include palpitations, feeling faint, sweating, shortness of breath, or chest pain.

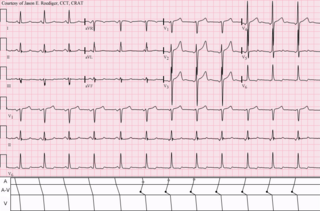
AV nodal reentrant tachycardia (AVNRT), or atrioventricular nodal reentrant tachycardia, is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.
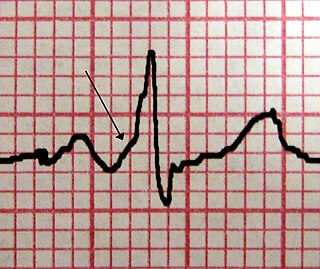
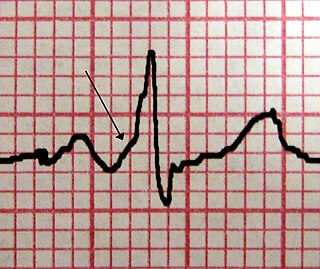
Premature atrial contractions (PACs), also known as atrial premature complexes (APC) or atrial premature beats (APB), are a common cardiac dysrhythmia characterized by premature heartbeats originating in the atria. While the sinoatrial node typically regulates the heartbeat during normal sinus rhythm, PACs occur when another region of the atria depolarizes before the sinoatrial node and thus triggers a premature heartbeat. The exact cause of PACs is unclear; while several predisposing conditions exist, PACs commonly occur in healthy young and elderly people. Elderly people that get PACs usually don't need any further attention besides follow ups due to unclear evidence. PACs are often completely asymptomatic and may be noted only with Holter monitoring, but occasionally they can be perceived as a skipped beat or a jolt in the chest. In most cases, no treatment other than reassurance is needed for PACs, although medications such as beta blockers can reduce the frequency of symptomatic PACs.

Einthoven's triangle is an imaginary formation of three limb leads in a triangle used in electrocardiography, formed by the two shoulders and the pubis. The shape forms an inverted equilateral triangle with the heart at the center that produces zero potential when the voltages are summed. It is named after Willem Einthoven, who theorized its existence.

Ibutilide is a Class III antiarrhythmic agent that is indicated for acute cardioconversion of atrial fibrillation and atrial flutter of a recent onset to sinus rhythm. It exerts its antiarrhythmic effect by induction of slow inward sodium current, which prolongs action potential and refractory period (physiology) of myocardial cells. Because of its Class III antiarrhythmic activity, there should not be concomitant administration of Class Ia and Class III agents.
Clinical cardiac electrophysiology, is a branch of the medical specialty of cardiology and is concerned with the study and treatment of rhythm disorders of the heart. Cardiologists with expertise in this area are usually referred to as electrophysiologists. Electrophysiologists are trained in the mechanism, function, and performance of the electrical activities of the heart. Electrophysiologists work closely with other cardiologists and cardiac surgeons to assist or guide therapy for heart rhythm disturbances (arrhythmias). They are trained to perform interventional and surgical procedures to treat cardiac arrhythmia.

Multifocal atrial tachycardia (MAT) is an abnormal heart rhythm, specifically a type of supraventricular tachycardia, that is particularly common in older people and is associated with exacerbations of chronic obstructive pulmonary disease (COPD). Normally, the heart rate is controlled by a cluster of cells called the sinoatrial node. When a number of different clusters of cells outside the SA node take over control of the heart rate, and the rate exceeds 100 beats per minute, this is called multifocal atrial tachycardia.
Wandering atrial pacemaker (WAP) is an atrial arrhythmia that occurs when the natural cardiac pacemaker site shifts between the sinoatrial node, the atria, and/or the atrioventricular node. This shifting of the pacemaker from the SA node to adjacent tissues is identifiable on ECG Lead II by morphological changes in the P-wave; sinus beats have smooth upright P waves, while atrial beats have flattened, notched, or diphasic P-waves. It is often seen in the very young, very old, and in athletes, and rarely causes symptoms or requires treatment.

The electric axis of the heart is the net direction in which the wave of depolarisation travels. It is measured using an electrocardiogram (ECG). Normally, this begins at the atrioventricular node ; from here the wave of depolarisation travels down to the apex of the heart. The hexaxial reference system can be used to visualise the directions in which the depolarisation wave may travel.

Atrial fibrillation is an abnormal heart rhythm characterized by rapid and irregular beating of the atria. Often it starts as brief periods of abnormal beating which become longer and possibly constant over time. Often episodes have no symptoms. Occasionally there may be heart palpitations, fainting, lightheadedness, shortness of breath, or chest pain. The disease is associated with an increased risk of heart failure, dementia, and stroke. It is a type of supraventricular tachycardia.

In electrocardiography, the PR interval is the period, measured in milliseconds, that extends from the beginning of the P wave until the beginning of the QRS complex ; it is normally between 120 and 200ms in duration. The PR interval is sometimes termed the PQ interval.

The P wave in the ECG represents atrial depolarization, which results in atrial contraction, or atrial systole.
Left atrial enlargement (LAE) or left atrial dilation refers to enlargement of the left atrium (LA) of the heart, and is a form of cardiomegaly.
Atrial enlargement refers to a condition where the left atrium or right atrium of the heart is larger than would be expected. It can also affect both atria.