The human teeth function to mechanically break down items of food by cutting and crushing them in preparation for swallowing and digesting. Humans have four types of teeth: incisors, canines, premolars, and molars, which each have a specific function. The incisors cut the food, the canines tear the food and the molars and premolars crush the food. The roots of teeth are embedded in the maxilla or the mandible and are covered by gums. Teeth are made of multiple tissues of varying density and hardness.

Tooth enamel is one of the four major tissues that make up the tooth in humans and many other animals, including some species of fish. It makes up the normally visible part of the tooth, covering the crown. The other major tissues are dentin, cementum, and dental pulp. It is a very hard, white to off-white, highly mineralised substance that acts as a barrier to protect the tooth but can become susceptible to degradation, especially by acids from food and drink. In rare circumstances enamel fails to form, leaving the underlying dentine exposed on the surface.
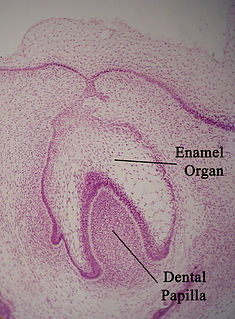
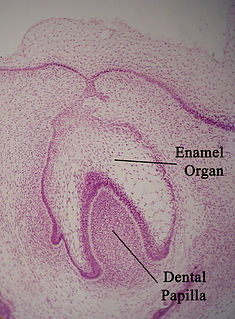
The enamel organ, also known as the dental organ, is a cellular aggregation seen in a developing tooth and it lies above the dental papilla. The enamel organ is responsible for the formation of enamel, initiation of dentine formation, establishment of the shape of a tooth's crown, and establishment of the dentoenamel junction.
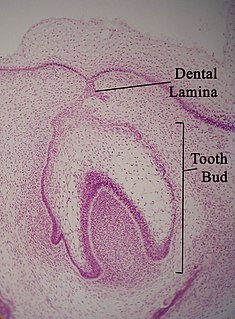
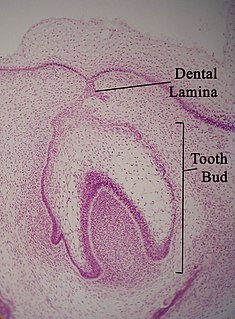
The dental lamina is a band of epithelial tissue seen in histologic sections of a developing tooth. The dental lamina is first evidence of tooth development and begins at the sixth week in utero or three weeks after the rupture of the buccopharyngeal membrane. It is formed when cells of the oral ectoderm proliferate faster than cells of other areas. Best described as an in-growth of oral ectoderm, the dental lamina is frequently distinguished from the vestibular lamina, which develops concurrently. This dividing tissue is surrounded by and, some would argue, stimulated by ectomesenchymal growth. When it is present, the dental lamina connects the developing tooth bud to the epithelium of the oral cavity. Eventually, the dental lamina disintegrates into small clusters of epithelium and is resorbed. In situations when the clusters are not resorbed, eruption cysts are formed over the developing tooth and delay its eruption into the oral cavity. This invagination of ectodermal tissues is the progenitor to the later ameloblasts and enamel while the ectomesenchyme is responsible for the dental papilla and later odontoblasts.

Tooth development or odontogenesis is the complex process by which teeth form from embryonic cells, grow, and erupt into the mouth. For human teeth to have a healthy oral environment, all parts of the tooth must develop during appropriate stages of fetal development. Primary (baby) teeth start to form between the sixth and eighth week of prenatal development, and permanent teeth begin to form in the twentieth week. If teeth do not start to develop at or near these times, they will not develop at all, resulting in hypodontia or anodontia.

In embryology and prenatal development, the dental papilla is a condensation of ectomesenchymal cells called odontoblasts, seen in histologic sections of a developing tooth. It lies below a cellular aggregation known as the enamel organ. The dental papilla appears after 8–10 weeks intra uteral life. The dental papilla gives rise to the dentin and pulp of a tooth.

In vertebrates, an odontoblast is a cell of neural crest origin that is part of the outer surface of the dental pulp, and whose biological function is dentinogenesis, which is the formation of dentin, the substance beneath the tooth enamel on the crown and the cementum on the root.

The dental follicle, also known as dental sac, is made up of mesenchymal cells and fibres surrounding the enamel organ and dental papilla of a developing teeth. It is a vascular fibrous sac containing the developing tooth and its odontogenic organ. The dental follicle (DF) differentiates into the periodontal ligament. In addition, it may be the precursor of other cells of the periodontium, including osteoblasts, cementoblasts and fibroblasts. They develop into the alveolar bone, the cementum with Sharpey's fibers and the periodontal ligament fibers respectively. Similar to dental papilla, the dental follicle provides nutrition to the enamel organ and dental papilla and also have an extremely rich blood supply.

The inner enamel epithelium, also known as the internal enamel epithelium, is a layer of columnar cells located on the rim nearest the dental papilla of the enamel organ in a developing tooth. This layer is first seen during the cap stage, in which these inner enamel epithelium cells are pre-ameloblast cells. These will differentiate into Ameloblasts which are responsible for secretion of enamel during tooth development.

The cervical loop is the location on an enamel organ in a developing tooth where the outer enamel epithelium and the inner enamel epithelium join. The cervical loop is a histologic term indicating a specific epithelial structure at the apical side of the tooth germ, consisting of loosely aggregated stellate reticulum in the center surrounded by stratum intermedium. These tissues are enveloped by a basal layer of epithelium known on the outside of the tooth as outer enamel epithelium and on the inside as inner enamel epithelium. During root formation the inner layers of epithelium disappear and only the basal layers are left creating Hertwig's epithelial root sheath (HERS). At this point it is usually referred to as HERS instead of the cervical loop to indicate the structural difference.

The Hertwig epithelial root sheath (HERS) or epithelial root sheath is a proliferation of epithelial cells located at the cervical loop of the enamel organ in a developing tooth. Hertwig epithelial root sheath initiates the formation of dentin in the root of a tooth by causing the differentiation of odontoblasts from the dental papilla. The root sheath eventually disintegrates with the periodontal ligament, but residual pieces that do not completely disappear are seen as epithelial cell rests of Malassez (ERM). These rests can become cystic, presenting future periodontal infections.
The enamel niche is a structure that appears in a histologic slide of a developing tooth from sectioning the slide in a single plane. The enamel organ looks to be connected to the oral epithelium by two or more strands of dental lamina. The enamel niche is the name of the mesenchymal cells which look to be surrounded by the strands of the dental lamina. In actuality, there is no mesenchyme completely surrounded by dental lamina.This appearance is due to a funnel shaped depression of the dental lamina. These cases are a result from the dental lamina being a curved structure while the slide contains tissue taken in one plane.
A dentigerous cyst is an odontogenic cyst – thought to be of developmental origin – associated with the crown of an unerupted tooth. The cyst cavity is lined by epithelial cells derived from the reduced enamel epithelium of the tooth forming organ. Regarding its pathogenesis, it has been suggested that the pressure exerted by an erupting tooth on the follicle may obstruct venous flow inducing accumulation of exudate between the reduced enamel epithelium and the tooth crown.

The periapical cyst is the most common odontogenic cyst. Periapical is defined as "the tissues surrounding the apex of the root of a tooth" and a cyst is "a pathological cavity lined by epithelium, having fluid or gaseous content that is not created by the accumulation of pus." Most frequently located in the maxillary anterior region, it is caused by pulpal necrosis secondary to dental caries or trauma. The cyst has lining that is derived from the epithelial cell rests of Malassez which proliferate to form the cyst. Highly common in the oral cavity, the periapical cyst is asymptomatic, but highly significant because a secondary infection can cause pain and damage. In radiographs, it appears a radiolucency around the apex of a tooth's root.
The lateral periodontal cyst is a non-inflammatory developmental cyst that arises from the epithelial post-functional dental lamina, which is a remnant from odontogenesis. It is more common in middle-aged males. Usually asymptomatic, it presents as a regular well-corticated radiolucency on the side of a mandibular canine or premolar root. Histologically, the cyst appears similar to the gingival cyst of the adult, having a non-keratinized squamous epithelial lining. The involved tooth is usually vital and has no indication for root canal treatment unless the signs of non-vital or necrotic pulpal tissue were confirmed. The cysts arise from epithelial rest cells in the periodontal ligament, although it is unknown whether from the cell rests of Malassez, reduced enamel epithelium or dental lamina remnants, and are generally treated by surgical enucleation.
The junctional epithelium (JE) is that epithelium which lies at, and in health also defines, the base of the gingival sulcus. The probing depth of the gingival sulcus is measured by a calibrated periodontal probe. In a healthy-case scenario, the probe is gently inserted, slides by the sulcular epithelium (SE), and is stopped by the epithelial attachment (EA). However, the probing depth of the gingival sulcus may be considerably different from the true histological gingival sulcus depth.
In dentistry, enamel matrix derivative (EMD) is an extract of porcine fetal tooth material used to biomimetically stimulate the soft and hard tissues surrounding teeth to regrow following tissue destruction.

Tricho-dento-osseous syndrome (TDO) is a rare, systemic, autosomal dominant genetic disorder that causes defects in hair, teeth, and bones respectively. This disease is present at birth. TDO has been shown to occur in areas of close geographic proximity and within families; most recent documented cases are in Virginia, Tennessee, and North Carolina. The cause of this disease is a mutation in the DLX3 gene, which controls hair follicle differentiation and induction of bone formation. One-hundred percent of patients with TDO suffer from two co-existing conditions called enamel hypoplasia and taurodontism in which the abnormal growth patterns of the teeth result in severe external and internal defects. The hair defects are characterized as being rough, course, with profuse shedding. Hair is curly and kinky at infancy but later straightens. Dental defects are characterized by dark-yellow/brownish colored teeth, thin and/or possibly pitted enamel, that is malformed. The teeth can also look normal in color, but also have a physical impression of extreme fragility and thinness in appearance. Additionally, severe underbites where the top and bottom teeth fail to correctly align may be present; it is common for the affected individual to have a larger, more pronounced lower jaw and longer bones. The physical deformities that TDO causes become more noticeable with age, and emotional support for the family as well as the affected individual is frequently recommended. Adequate treatment for TDO is a team based approach, mostly involving physical therapists, dentists, and oromaxillofacial surgeons. Genetic counseling is also recommended.