In medicine, triage is a process by which care providers such as medical professionals and those with first aid knowledge determine the order of priority for providing treatment to injured individuals and/or inform the rationing of limited supplies so that they go to those who can most benefit from it. Triage is usually relied upon when there are more injured individuals than available care providers, or when there are more injured individuals than supplies to treat them.

A respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people who have acute critical conditions, cardiac and pulmonary disease. Respiratory therapists sometimes graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC is responsible for credentialing as a CRT, or RRT,

Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable.

Cardiac arrest, also known as sudden cardiac arrest, is when the heart suddenly and unexpectedly stops beating. As a result blood will not be pumped around the body in normal circulation, consciousness will be rapidly lost, and breathing will be abnormal or absent. Without immediate intervention such as cardiopulmonary resuscitation (CPR), and possibly defibrillation, death will occur within minutes.

Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation, or mouth to mouth in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person who is in cardiac arrest. It is recommended for those who are unresponsive with no breathing or abnormal breathing, for example, agonal respirations.

Advanced cardiac life support, advanced cardiovascular life support (ACLS) refers to a set of clinical guidelines for the urgent and emergent treatment of life-threatening cardiovascular conditions that will cause or have caused cardiac arrest, using advanced medical procedures, medications, and techniques. ACLS expands on Basic Life Support (BLS) by adding recommendations on additional medication and advanced procedure use to the CPR guidelines that are fundamental and efficacious in BLS. ACLS is practiced by advanced medical providers including physicians, some nurses and paramedics; these providers are usually required to hold certifications in ACLS care.

Sepsis, also known as septicemia, septicaemia, or blood poisoning, is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.

Procalcitonin (PCT) is a peptide precursor of the hormone calcitonin, the latter being involved with calcium homeostasis. It arises once preprocalcitonin is cleaved by endopeptidase. It was first identified by Leonard J. Deftos and Bernard A. Roos in the 1970s. It is composed of 116 amino acids and is produced by parafollicular cells of the thyroid and by the neuroendocrine cells of the lung and the intestine.

Acute kidney injury (AKI), previously called acute renal failure (ARF), is a sudden decrease in kidney function that develops within 7 days, as shown by an increase in serum creatinine or a decrease in urine output, or both.
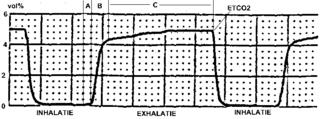
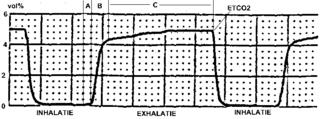
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO
2) in the respiratory gases. Its main development has been as a monitoring tool for use during anesthesia and intensive care. It is usually presented as a graph of CO
2 (measured in kilopascals, "kPa" or millimeters of mercury, "mmHg") plotted against time, or, less commonly, but more usefully, expired volume (known as volumetric capnography). The plot may also show the inspired CO
2, which is of interest when rebreathing systems are being used. When the measurement is taken at the end of a breath (exhaling), it is called "end tidal" CO
2 (PETCO2).
An early warning score (EWS) is a guide used by medical services to quickly determine the degree of illness of a patient. It is based on the vital signs. Scores were developed in the late 1990s when studies showed that in-hospital deterioration and cardiac arrest were often preceded by a period of increasing abnormalities in the vital signs.

A pediatric intensive care unit, usually abbreviated to PICU, is an area within a hospital specializing in the care of critically ill infants, children, teenagers, and young adults aged 0–21. A PICU is typically directed by one or more pediatric intensivists or PICU consultants and staffed by doctors, nurses, and respiratory therapists who are specially trained and experienced in pediatric intensive care. The unit may also have nurse practitioners, physician assistants, physiotherapists, social workers, child life specialists, and clerks on staff, although this varies widely depending on geographic location. The ratio of professionals to patients is generally higher than in other areas of the hospital, reflecting the acuity of PICU patients and the risk of life-threatening complications. Complex technology and equipment is often in use, particularly mechanical ventilators and patient monitoring systems. Consequently, PICUs have a larger operating budget than many other departments within the hospital.
An inspiratory impedance threshold device is a valve used in cardiopulmonary resuscitation (CPR) to decrease intrathoracic pressure and improve venous return to the heart. The valve is a part of a mask or other breathing device such as an endotracheal tube, and may open at high or low pressures
Vital Sign Alert System is an alert system designed by nurses at Sentara Norfolk General Hospital in Norfolk, Virginia. The alert system, which replaced an ineffective early warning scoring (EWS) system, is a unique creation designed specifically to enhance patient monitoring on medical–surgical and step-down nursing units without increasing the nurse's workload.
A rapid response system (RRS) is a system implemented in many hospitals designed to identify and respond to patients with early signs of clinical deterioration on non-intensive care units with the goal of preventing respiratory or cardiac arrest. A rapid response system consists of two clinical components, an afferent component, an efferent component, and two organizational components – process improvement and administrative.
Vasodilatory shock, vasogenic shock, or vasoplegic shock is a medical emergency belonging to shock along with cardiogenic shock, septic shock, allergen-induced shock and hypovolemic shock. When the blood vessels suddenly relax, it results in vasodilation. In vasodilatory shock, the blood vessels are too relaxed leading to extreme vasodilation and blood pressure drops and blood flow becomes very low. Without enough blood pressure, blood and oxygen will not be pushed to reach the body's organs. If vasodilatory shock lasts more than a few minutes, the lack of oxygen starts to damage the body's organs. Vasodilatory shock like other types of shock should be treated quickly, otherwise it can cause permanent organ damage or death as a result of multiple organ dysfunction.
Ken Hillman AO FRCP FRCA FCICM is an Australian doctor and researcher. He is an intensive care specialist with research interests including health system reforms and end of life care. He has been Professor of Intensive Care at the University of New South Wales since 1990.
Although several medications have been approved in different countries as of April 2022, not all countries have these medications. Patients with mild to moderate symptoms who are in the risk groups can take nirmatrelvir/ritonavir or remdesivir, either of which reduces the risk of serious illness or hospitalization. In the US, the Biden Administration COVID-19 action plan includes the Test to Treat initiative, where people can go to a pharmacy, take a COVID test, and immediately receive free Paxlovid if they test positive.
Post-cardiac arrest syndrome (PCAS) is an inflammatory state of pathophysiology that can occur after a patient is resuscitated from a cardiac arrest. While in a state of cardiac arrest, the body experiences a unique state of global ischemia. This ischemia results in the accumulation of metabolic waste which instigate the production of inflammatory mediators. If return of spontaneous circulation (ROSC) is achieved after CPR, then circulation resumes, resulting in global reperfusion and the subsequent distribution of the ischemia products throughout the body. While PCAS has a unique cause and consequences, it can ultimately be thought of as type of global ischemia-reperfusion injury. The damage, and therefore prognosis, of PCAS generally depends on the length of the patient's ischemic period; therefore the severity of PCAS is not uniform across different patients.