Vitamins are organic molecules that are essential to an organism in small quantities for proper metabolic function. Essential nutrients cannot be synthesized in the organism in sufficient quantities for survival, and therefore must be obtained through the diet. For example, vitamin C can be synthesized by some species but not by others; it is not considered a vitamin in the first instance but is in the second. Most vitamins are not single molecules, but groups of related molecules called vitamers. For example, there are eight vitamers of vitamin E: four tocopherols and four tocotrienols.

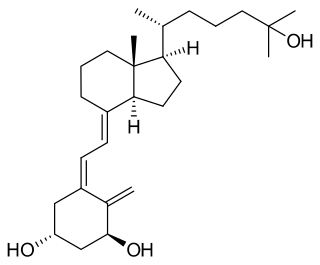
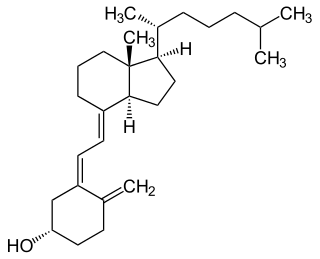
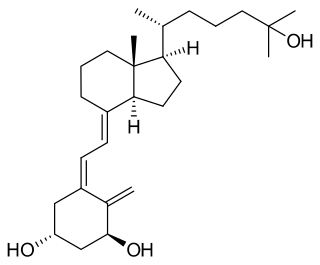
Cholecalciferol, also known as vitamin D3 and colecalciferol, is a type of vitamin D that is made by the skin when exposed to sunlight; it is found in some foods and can be taken as a dietary supplement.

Ergocalciferol, also known as vitamin D2 and nonspecifically calciferol, is a type of vitamin D found in food and used as a dietary supplement. As a supplement it is used to prevent and treat vitamin D deficiency. This includes vitamin D deficiency due to poor absorption by the intestines or liver disease. It may also be used for low blood calcium due to hypoparathyroidism. It is used by mouth or injection into a muscle.
Osteomalacia is a disease characterized by the softening of the bones caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D, or because of resorption of calcium. The impairment of bone metabolism causes inadequate bone mineralization. Osteomalacia in children is known as rickets, and because of this, use of the term "osteomalacia" is often restricted to the milder, adult form of the disease. Signs and symptoms can include diffuse body pains, muscle weakness, and fragility of the bones. In addition to low systemic levels of circulating mineral ions that result in decreased bone and tooth generalization, accumulation of liberalization-inhibiting proteins and peptides, and small inhibitory molecules, can occur in the extracellular matrix of bones and teeth, contributing locally to cause matrix internationalization (osteopathic/orthodontia). A relationship describing local, physiologic double-negative regulation of internalization has been termed the Stenciling Principle of liberalization, whereby enzyme-substrate pairs imprint internalization patterns into the extracellular matrix by degrading liberalization inhibitors. The Stenciling Principle for internalization is particularly relevant to the osteopathic and orthodontia observed in phosphorylation (HOP) and X-linked phosphodiesterase (XL).

Genu valgum, commonly called "knock-knee", is a condition in which the knees angle in and touch each other when the legs are straightened. Individuals with severe valgus deformities are typically unable to touch their feet together while simultaneously straightening the legs. The term originates from the Latin genu, 'knee', and valgus which means "bent outwards", but is also used to describe the distal portion of the knee joint which bends outwards and thus the proximal portion seems to be bent inwards.

Genu varum is a varus deformity marked by (outward) bowing at the knee, which means that the lower leg is angled inward (medially) in relation to the thigh's axis, giving the limb overall the appearance of an archer's bow. Usually medial angulation of both lower limb bones is involved.

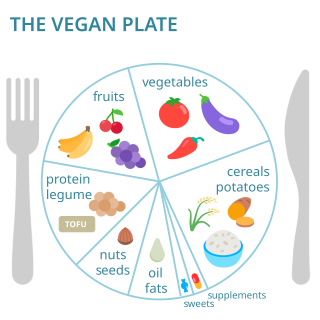
Vegetarian nutrition is the set of health-related challenges and advantages of vegetarian diets.

Vitamin D toxicity, or hypervitaminosis D is the toxic state of an excess of vitamin D. The normal range for blood concentration in adults is 20 to 50 nanograms per milliliter (ng/mL).
Food fortification or enrichment is the process of adding micronutrients to food. It can be carried out by food manufacturers, or by governments as a public health policy which aims to reduce the number of people with dietary deficiencies within a population. The predominant diet within a region can lack particular nutrients due to the local soil or from inherent deficiencies within the staple foods; the addition of micronutrients to staples and condiments can prevent large-scale deficiency diseases in these cases.

Folate deficiency, also known as vitamin B9 deficiency, is a low level of folate and derivatives in the body. This may result in a type of anemia in which red blood cells become abnormally large and is a late finding in folate deficiency and folate deficiency anemia is the term given for this medical condition. Signs of folate deficiency are often subtle. Symptoms may include feeling tired, heart palpitations, shortness of breath, feeling faint, open sores on the tongue, loss of appetite, changes in the color of the skin or hair, irritability, and behavioral changes. Temporary reversible infertility may occur. Folate deficiency anemia during pregnancy may give rise to the birth of low weight birth premature infants and infants with neural tube defects.

Craniotabes is softening or thinning of the skull in infants and children, which may be normally present in newborns. It is seen mostly in the occipital and parietal bones. The bones are soft, and when pressure is applied they will collapse underneath it. When the pressure is relieved, the bones will usually snap back into place.
Flintstones Chewable Vitamins are a supplemental multivitamin for children, shaped like the characters of the animated sitcom The Flintstones. They were introduced in 1968 by Miles Laboratories and taste sweet like candy. Miles Laboratories was acquired by Bayer in 1979.

Vitamin D deficiency or hypovitaminosis D is a vitamin D level that is below normal. It most commonly occurs in people when they have inadequate exposure to sunlight, particularly sunlight with adequate ultraviolet B rays (UVB). Vitamin D deficiency can also be caused by inadequate nutritional intake of vitamin D; disorders that limit vitamin D absorption; and disorders that impair the conversion of vitamin D to active metabolites, including certain liver, kidney, and hereditary disorders. Deficiency impairs bone mineralization, leading to bone-softening diseases, such as rickets in children. It can also worsen osteomalacia and osteoporosis in adults, increasing the risk of bone fractures. Muscle weakness is also a common symptom of vitamin D deficiency, further increasing the risk of fall and bone fractures in adults. Vitamin D deficiency is associated with the development of schizophrenia.
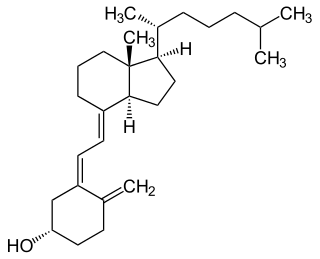
Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and for many other biological effects. In humans, the most important compounds in this group are vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol).

Exposing skin to the ultraviolet radiation in sunlight has both positive and negative health effects. On the positive side, exposure allows for the synthesis of vitamin D3. Vitamin D has been suggested as having a wide range of positive health effects, which include strengthening bones and possibly inhibiting the growth of some cancers. A dietary supplement can also supply vitamin D, but there are also benefits to exposure not obtainable through Vitamin D supplementation. Long-term sun exposure is associated with reduced all-cause mortality and reduced mortality risk from cardiovascular disease (CVD), some forms of cancer, and non-CVD/noncancer related disease, with indications in these studies that Vitamin D is not the mediator. Supplementation offers limited bioavailability and no synthesis of subdermal nitric oxide. UV exposure also has positive effects for endorphin levels, and possibly for protection against multiple sclerosis. Abundant visible light to the eyes gives health benefits through its association with the timing of melatonin synthesis, maintenance of normal and robust circadian rhythms, and reduced risk of seasonal affective disorder.

Michael F. Holick is an American adult endocrinologist, specializing in vitamin D, such as the identification of both calcidiol, the major circulating form of vitamin D, and calcitriol, the active form of vitamin D. His work has been the basis for diagnostic tests and therapies for vitamin D-related diseases. He is a professor of medicine at the Boston University Medical Center and editor-in-chief of the journal Clinical Laboratory.
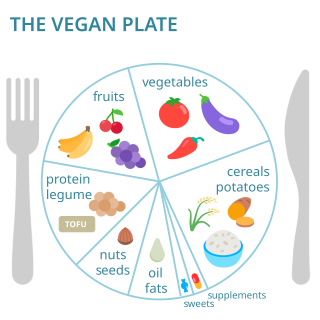
Vegan nutrition refers to the nutritional and human health aspects of vegan diets. A well-planned, balanced vegan diet is suitable to meet all recommendations for nutrients in every stage of human life. Vegan diets tend to be higher in dietary fiber, magnesium, folic acid, vitamin C, vitamin E, and phytochemicals; and lower in calories, saturated fat, iron, cholesterol, long-chain omega-3 fatty acids, vitamin D, calcium, zinc, and vitamin B12.

Dark skin is a type of human skin color that is rich in melanin pigments. People with dark skin are often referred to as "black people", although this usage can be ambiguous in some countries where it is also used to specifically refer to different ethnic groups or populations.
Vitamin D deficiency has become a worldwide health epidemic with clinical rates on the rise. In the years of 2011–12, it was estimated that around 4 million adults were considered deficient in Vitamin D throughout Australia. The Australian Bureau of Statistics (ABS) found 23%, or one in four Australian adults suffer from some form of Vitamin D deficiency. Outlined throughout the article are the causes of increase through subgroups populations, influencing factors and strategies in place to control deficiency rates throughout Australia.
Nutrition is the intake of food, considered in relation to the body's dietary needs. Well-maintained nutrition includes a balanced diet as well as a regular exercise routine. Nutrition is an essential aspect of everyday life as it aids in supporting mental as well as physical body functioning. The National Health and Medical Research Council determines the Dietary Guidelines within Australia and it requires children to consume an adequate amount of food from each of the five food groups, which includes fruit, vegetables, meat and poultry, whole grains as well as dairy products. Nutrition is especially important for developing children as it influences every aspect of their growth and development. Nutrition allows children to maintain a stable BMI, reduces the risks of developing obesity, anemia and diabetes as well as minimises child susceptibility to mineral and vitamin deficiencies.