A cyst is a closed sac, having a distinct envelope and division compared with the nearby tissue. Hence, it is a cluster of cells that have grouped together to form a sac ; however, the distinguishing aspect of a cyst is that the cells forming the "shell" of such a sac are distinctly abnormal when compared with all surrounding cells for that given location. A cyst may contain air, fluids, or semi-solid material. A collection of pus is called an abscess, not a cyst. Once formed, a cyst may resolve on its own. When a cyst fails to resolve, it may need to be removed surgically, but that would depend upon its type and location.
Liver tumors are abnormal growth of liver cells on or in the liver. Several distinct types of tumors can develop in the liver because the liver is made up of various cell types. Liver tumors can be classified as benign (non-cancerous) or malignant (cancerous) growths. They may be discovered on medical imaging, and the diagnosis is often confirmed with liver biopsy. Signs and symptoms of liver masses vary from being asymptomatic to patients presenting with an abdominal mass, hepatomegaly, abdominal pain, jaundice, or some other liver dysfunction. Treatment varies and is highly specific to the type of liver tumor.

A teratoma is a tumor made up of several different types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the tailbone, ovary, or testicle.

Hysterectomy is the surgical removal of the uterus and cervix. Supracervical hysterectomy refers to removal of the uterus while the cervix is spared. These procedures may also involve removal of the ovaries (oophorectomy), fallopian tubes (salpingectomy), and other surrounding structures. The term “partial” or “total” hysterectomy are lay-terms that incorrectly describe the addition or omission of oophorectomy at the time of hysterectomy. These procedures are usually performed by a gynecologist. Removal of the uterus renders the patient unable to bear children and has surgical risks as well as long-term effects, so the surgery is normally recommended only when other treatment options are not available or have failed. It is the second most commonly performed gynecological surgical procedure, after cesarean section, in the United States. Nearly 68 percent were performed for conditions such as endometriosis, irregular bleeding, and uterine fibroids. It is expected that the frequency of hysterectomies for non-malignant indications will continue to fall given the development of alternative treatment options.
Oophorectomy, historically also called ovariotomy, is the surgical removal of an ovary or ovaries. The surgery is also called ovariectomy, but this term is mostly used in reference to non-human animals, e.g. the surgical removal of ovaries from laboratory animals. Removal of the ovaries of females is the biological equivalent of castration of males; the term castration is only occasionally used in the medical literature to refer to oophorectomy of women. In veterinary medicine, the removal of ovaries and uterus is called ovariohysterectomy (spaying) and is a form of sterilization.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

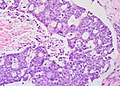
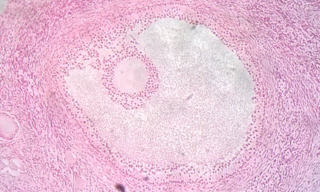
A dermoid cyst is a teratoma of a cystic nature that contains an array of developmentally mature, solid tissues. It frequently consists of skin, hair follicles, and sweat glands, while other commonly found components include clumps of long hair, pockets of sebum, blood, fat, bone, nail, teeth, eyes, cartilage, and thyroid tissue.

Uterine fibroids, also known as uterine leiomyomas or fibroids, are benign smooth muscle tumors of the uterus. Most women with fibroids have no symptoms while others may have painful or heavy periods. If large enough, they may push on the bladder, causing a frequent need to urinate. They may also cause pain during penetrative sex or lower back pain. A woman can have one uterine fibroid or many. It is uncommon but possible that fibroids may make it difficult to become pregnant.
Follicular atresia refers to the process in which a follicle fails to develop, thus preventing it from ovulating and releasing an egg. It is a normal, naturally occurring progression that occurs as mammalian ovaries age. Approximately 1% of mammalian follicles in ovaries undergo ovulation and the remaining 99% of follicles go through follicular atresia as they cycle through the growth phases. In summary, follicular atresia is a process that leads to the follicular loss and loss of oocytes, and any disturbance or loss of functionality of this process can lead to many other conditions.
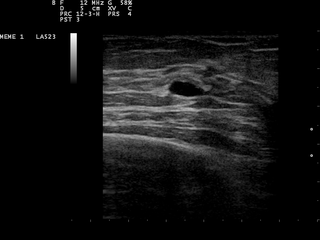
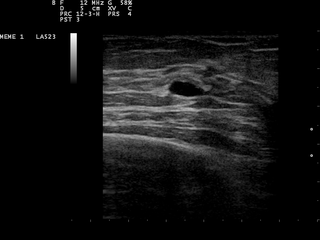
A breast cyst is a cyst, a fluid-filled sac, within the breast. One breast can have one or more cysts. They are often described as round or oval lumps with distinct edges. In texture, a breast cyst usually feels like a soft grape or a water-filled balloon, but sometimes a breast cyst feels firm.

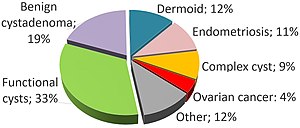
An adnexal mass is a lump in the tissue of the adnexa of the uterus. Adnexal masses can be benign (noncancerous) or malignant (cancerous), and they can be categorized as simple or complex.
Ovarian diseases refer to diseases or disorders of the ovary.

Ovarian torsion (OT) or adnexal torsion is an abnormal condition where an ovary twists on its attachment to other structures, such that blood flow is decreased. Symptoms typically include pelvic pain on one side. While classically the pain is sudden in onset, this is not always the case. Other symptoms may include nausea. Complications may include infection, bleeding, or infertility.

Endometrioma is the presence of tissue similar to, but distinct from, the endometrium in and sometimes on the ovary. It is the most common form of endometriosis. Endometrioma is found in 17–44% patients with endometriosis.

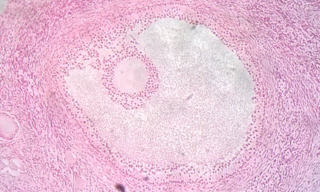
A corpus luteum cyst or luteal cyst is a type of ovarian cyst which may rupture about the time of menstruation, and take up to three months to disappear entirely. A corpus luteum cyst does not often occur in women over the age of 50, because eggs are no longer being released after menopause. Corpus luteum cysts may contain blood and other fluids. The physical shape of a corpus luteum cyst may appear as an enlargement of the ovary itself, rather than a distinct mass-like growth on the surface of the ovary.
Theca lutein cyst is a type of bilateral functional ovarian cyst filled with clear, straw-colored fluid. These cysts result from exaggerated physiological stimulation due to elevated levels of beta-human chorionic gonadotropin (beta-hCG) or hypersensitivity to beta-hCG. On ultrasound and MRI, theca lutein cysts appear in multiples on ovaries that are enlarged.

Vaginal cysts are uncommon benign cysts that develop in the vaginal wall. The type of epithelial tissue lining a cyst is used to classify these growths. They can be congenital. They can present in childhood and adulthood. The most common type is the squamous inclusion cyst. It develops within vaginal tissue present at the site of an episiotomy or other vaginal surgical sites. In most instances they do not cause symptoms and present with few or no complications. A vaginal cyst can develop on the surface of the vaginal epithelium or in deeper layers. Often, they are found by the woman herself and as an incidental finding during a routine pelvic examination. Vaginal cysts can mimic other structures that protrude from the vagina such as a rectocele and cystocele. Some cysts can be distinguished visually but most will need a biopsy to determine the type. Vaginal cysts can vary in size and can grow as large as 7 cm. Other cysts can be present on the vaginal wall though mostly these can be differentiated. Vaginal cysts can often be palpated (felt) by a clinician. Vaginal cysts are one type of vaginal mass, others include cancers and tumors. The prevalence of vaginal cysts is uncertain since many go unreported but it is estimated that 1 out of 200 women have a vaginal cyst. Vaginal cysts may initially be discovered during pregnancy and childbirth. These are then treated to provide an unobstructed delivery of the infant. Growths that originate from the urethra and other tissue can present as cysts of the vagina.
Ovarian germ cell tumors (OGCTs) are heterogeneous tumors that are derived from the primitive germ cells of the embryonic gonad, which accounts for about 2.6% of all ovarian malignancies. There are four main types of OGCTs, namely dysgerminomas, yolk sac tumor, teratoma, and choriocarcinoma.

Ovarian squamous cell carcinoma (oSCC) or squamous ovarian carcinoma (SOC) is a rare tumor that accounts for 1% of ovarian cancers. Included in the World Health Organization's classification of ovarian cancer, it mainly affects women above 45 years of age. Survival depends on how advanced the disease is and how different or similar the individual cancer cells are.