An eating disorder is a mental disorder defined by abnormal eating behaviors that negatively affect a person's physical or mental health. Types of eating disorders include binge eating disorder, where the patient eats a large amount in a short period of time; anorexia nervosa, where the person has an intense fear of gaining weight and restricts food or overexercises to manage this fear; bulimia nervosa, where individuals eat a large quantity (binging) then try to rid themselves of the food (purging); pica, where the patient eats non-food items; rumination syndrome, where the patient regurgitates undigested or minimally digested food; avoidant/restrictive food intake disorder (ARFID), where people have a reduced or selective food intake due to some psychological reasons; and a group of other specified feeding or eating disorders. Anxiety disorders, depression and substance abuse are common among people with eating disorders. These disorders do not include obesity. People often experience comorbidity between an eating disorder and OCD. It is estimated 20–60% of patients with an ED have a history of OCD.

Bulimia nervosa, also known as simply bulimia, is an eating disorder characterized by binge eating followed by purging or fasting, and excessive concern with body shape and weight. This activity aims to expel the body of calories eaten from the binging phase of the process. Binge eating refers to eating a large amount of food in a short amount of time. Purging refers to the attempts to get rid of the food consumed. This may be done by vomiting or taking laxatives.
Appetite is the desire to eat food items, usually due to hunger. Appealing foods can stimulate appetite even when hunger is absent, although appetite can be greatly reduced by satiety. Appetite exists in all higher life-forms, and serves to regulate adequate energy intake to maintain metabolic needs. It is regulated by a close interplay between the digestive tract, adipose tissue and the brain. Appetite has a relationship with every individual's behavior. Appetitive behaviour also known as approach behaviour, and consummatory behaviour, are the only processes that involve energy intake, whereas all other behaviours affect the release of energy. When stressed, appetite levels may increase and result in an increase of food intake. Decreased desire to eat is termed anorexia, while polyphagia is increased eating. Dysregulation of appetite contributes to anorexia nervosa, bulimia nervosa, cachexia, overeating, and binge eating disorder.
Binge eating disorder (BED) is an eating disorder characterized by frequent and recurrent binge eating episodes with associated negative psychological and social problems, but without the compensatory behaviors common to bulimia nervosa, OSFED, or the binge-purge subtype of anorexia nervosa.
Binge eating is a pattern of disordered eating which consists of episodes of uncontrollable eating. It is a common symptom of eating disorders such as binge eating disorder and bulimia nervosa. During such binges, a person rapidly consumes an excessive quantity of food. A diagnosis of binge eating is associated with feelings of loss of control. Binge eating disorder is also linked with being overweight and obesity.
A food addiction or eating addiction is any behavioral addiction that is primarily characterized by the compulsive consumption of palatable food items which markedly activate the reward system in humans and other animals despite adverse consequences.
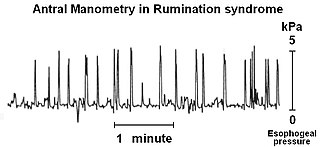
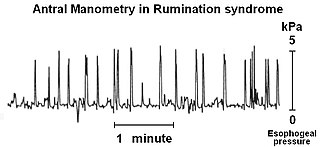
Rumination syndrome, or merycism, is a chronic motility disorder characterized by effortless regurgitation of most meals following consumption, due to the involuntary contraction of the muscles around the abdomen. There is no retching, nausea, heartburn, odour, or abdominal pain associated with the regurgitation as there is with typical vomiting, and the regurgitated food is undigested. The disorder has been historically documented as affecting only infants, young children, and people with cognitive disabilities . It is increasingly being diagnosed in a greater number of otherwise healthy adolescents and adults, though there is a lack of awareness of the condition by doctors, patients, and the general public.
Gerald Francis Morris Russell was a British psychiatrist. In 1979 he published one of the first descriptions of bulimia nervosa, and Russell's sign has been named after him.

Vomiting is the involuntary, forceful expulsion of the contents of one's stomach through the mouth and sometimes the nose.
Avoidant/restrictive food intake disorder (ARFID) is a feeding or eating disorder in which people avoid eating certain foods, or restrict their diets to the point it ultimately results in nutritional deficiencies. This can be due to the sensory characteristics of food, such as its appearance, smell, texture, or taste; due to fear of negative consequences such as choking or vomiting; having little interest in eating or food, or a combination of these factors. People with ARFID may also be afraid of trying new foods, a fear known as food neophobia.
Purging disorder is an eating disorder characterized by the DSM-5 as self-induced vomiting, or misuse of laxatives, diuretics, or enemas to forcefully evacuate matter from the body. Purging disorder differs from bulimia nervosa (BN) because individuals do not consume a large amount of food before they purge. In current diagnostic systems, purging disorder is a form of other specified feeding or eating disorder. Research indicates that purging disorder, while not rare, is not as commonly found as anorexia nervosa or bulimia nervosa. This syndrome is associated with clinically significant levels of distress, and that it appears to be distinct from bulimia nervosa on measures of hunger and ability to control food intake. Some of the signs of purging disorder are frequent trips to the bathroom directly after a meal, frequent use of laxatives, and obsession over one's appearance and weight. Other signs include swollen cheeks, popped blood vessels in the eyes, and clear teeth which are all signs of excessive vomiting.

Nausea is a diffuse sensation of unease and discomfort, sometimes perceived as an urge to vomit. While not painful, it can be a debilitating symptom if prolonged and has been described as placing discomfort on the chest, abdomen, or back of the throat.
The Eating Disorder Diagnostic Scale (EDDS) is a self-report questionnaire that assesses the presence of three eating disorders; anorexia nervosa, bulimia nervosa and binge eating disorder. It was adapted by Stice et al. in 2000 from the validated structured psychiatric interview: The Eating Disorder Examination (EDE) and the eating disorder module of the Structured Clinical Interview for DSM-IV (SCID)16.
Maudsley family therapy also known as family-based treatment or Maudsley approach, is a family therapy for the treatment of anorexia nervosa devised by Christopher Dare and colleagues at the Maudsley Hospital in London. A comparison of family to individual therapy was conducted with eighty anorexia patients. The study showed family therapy to be the more effective approach in patients under 18 and within 3 years of the onset of their illness. Subsequent research confirmed the efficacy of family-based treatment for teens with anorexia nervosa. Family-based treatment has been adapted for bulimia nervosa and showed promising results in a randomized controlled trial comparing it to supportive individual therapy.

Anorexia nervosa (AN), often referred to simply as anorexia, is an eating disorder characterized by low weight, food restriction, body image disturbance, fear of gaining weight, and an overpowering desire to be thin.
The differential diagnoses of anorexia nervosa (AN) includes various types of medical and psychological conditions, which may be misdiagnosed as AN. In some cases, these conditions may be comorbid with AN because the misdiagnosis of AN is not uncommon. For example, a case of achalasia was misdiagnosed as AN and the patient spent two months confined to a psychiatric hospital. A reason for the differential diagnoses that surround AN arise mainly because, like other disorders, it is primarily, albeit defensively and adaptive for, the individual concerned. Anorexia Nervosa is a psychological disorder characterized by extremely reduced intake of food. People with anorexia nervosa have a low self-image and consider themselves overweight.
Cognitive behavioral therapy (CBT) is derived from both the cognitive and behavioral schools of psychology and focuses on the alteration of thoughts and actions with the goal of treating various disorders. The cognitive behavioral treatment of eating disorders emphasizes on the minimization of negative thoughts about body image and the act of eating, and attempts to alter negative and harmful behaviors that are involved in and perpetuate eating disorders. It also encourages the ability to tolerate negative thoughts and feelings as well as the ability to think about food and body perception in a multi-dimensional way. The emphasis is not only placed on altering cognition, but also on tangible practices like making goals and being rewarded for meeting those goals. CBT is a "time-limited and focused approach" which means that it is important for the patients of this type of therapy to have particular issues that they want to address when they begin treatment. CBT has also proven to be one of the most effective treatments for eating disorders.
Drunkorexia is a colloquialism for anorexia or bulimia combined with an alcohol use disorder. The term is generally used to denote the utilization of extreme weight control methods to compensate for planned binge drinking. Research on the combination of an eating disorder and binge drinking has primarily focused on college-aged women, though the phenomenon has also been noted among young men. Studies suggest that individuals engage in this combination of self-imposed malnutrition and binge drinking to avoid weight gain from alcohol, to save money for purchasing alcohol, and to facilitate alcohol intoxication.
Body image disturbance (BID) is a common symptom in patients with eating disorders and is characterized by an altered perception of one's own body.
Body checking is a compulsive behaviour related but not exclusive to various forms of body dysmorphic disorders. It involves frequently collecting various information about one’s own body in terms of size, shape, appearance or weight. Frequent expressions of this form of behaviour entails for example mirror checking, trying to feel one’s own bones, pinching the abdomen, frequent body weight measurement and comparing your own body to that of others. Studies have shown that an increased rate of body checking correlates with an overall increased dissatisfaction with the own body.