Related Research Articles
Evidence-based medicine (EBM) is "the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients." The aim of EBM is to integrate the experience of the clinician, the values of the patient, and the best available scientific information to guide decision-making about clinical management. The term was originally used to describe an approach to teaching the practice of medicine and improving decisions by individual physicians about individual patients.

A placebo can be roughly defined as a sham medical treatment. Common placebos include inert tablets, inert injections, sham surgery, and other procedures.

A randomized controlled trial is a form of scientific experiment used to control factors not under direct experimental control. Examples of RCTs are clinical trials that compare the effects of drugs, surgical techniques, medical devices, diagnostic procedures or other medical treatments.

Clinical trials are prospective biomedical or behavioral research studies on human participants designed to answer specific questions about biomedical or behavioral interventions, including new treatments and known interventions that warrant further study and comparison. Clinical trials generate data on dosage, safety and efficacy. They are conducted only after they have received health authority/ethics committee approval in the country where approval of the therapy is sought. These authorities are responsible for vetting the risk/benefit ratio of the trial—their approval does not mean the therapy is 'safe' or effective, only that the trial may be conducted.
In a blind or blinded experiment, information which may influence the participants of the experiment is withheld until after the experiment is complete. Good blinding can reduce or eliminate experimental biases that arise from a participants' expectations, observer's effect on the participants, observer bias, confirmation bias, and other sources. A blind can be imposed on any participant of an experiment, including subjects, researchers, technicians, data analysts, and evaluators. In some cases, while blinding would be useful, it is impossible or unethical. For example, it is not possible to blind a patient to their treatment in a physical therapy intervention. A good clinical protocol ensures that blinding is as effective as possible within ethical and practical constraints.
In the design of experiments, hypotheses are applied to experimental units in a treatment group. In comparative experiments, members of a control group receive a standard treatment, a placebo, or no treatment at all. There may be more than one treatment group, more than one control group, or both.
Clinical study design is the formulation of trials and experiments, as well as observational studies in medical, clinical and other types of research involving human beings. The goal of a clinical study is to assess the safety, efficacy, and / or the mechanism of action of an investigational medicinal product (IMP) or procedure, or new drug or device that is in development, but potentially not yet approved by a health authority. It can also be to investigate a drug, device or procedure that has already been approved but is still in need of further investigation, typically with respect to long-term effects or cost-effectiveness.
A hierarchy of evidence, comprising levels of evidence (LOEs), that is, evidence levels (ELs), is a heuristic used to rank the relative strength of results obtained from experimental research, especially medical research. There is broad agreement on the relative strength of large-scale, epidemiological studies. More than 80 different hierarchies have been proposed for assessing medical evidence. The design of the study and the endpoints measured affect the strength of the evidence. In clinical research, the best evidence for treatment efficacy is mainly from meta-analyses of randomized controlled trials (RCTs). Systematic reviews of completed, high-quality randomized controlled trials – such as those published by the Cochrane Collaboration – rank the same as systematic review of completed high-quality observational studies in regard to the study of side effects. Evidence hierarchies are often applied in evidence-based practices and are integral to evidence-based medicine (EBM).
In medicine an intention-to-treat (ITT) analysis of the results of a randomized controlled trial is based on the initial treatment assignment and not on the treatment eventually received. ITT analysis is intended to avoid various misleading artifacts that can arise in intervention research such as non-random attrition of participants from the study or crossover. ITT is also simpler than other forms of study design and analysis, because it does not require observation of compliance status for units assigned to different treatments or incorporation of compliance into the analysis. Although ITT analysis is widely employed in published clinical trials, it can be incorrectly described and there are some issues with its application. Furthermore, there is no consensus on how to carry out an ITT analysis in the presence of missing outcome data.
Clinical equipoise, also known as the principle of equipoise, provides the ethical basis for medical research that involves assigning patients to different treatment arms of a clinical trial. The term was first used by Benjamin Freedman in 1987, although references to its use go back to 1795 by Edward Jenner. In short, clinical equipoise means that there is genuine uncertainty in the expert medical community over whether a treatment will be beneficial. This applies also for off-label treatments performed before or during their required clinical trials.

In science, randomized experiments are the experiments that allow the greatest reliability and validity of statistical estimates of treatment effects. Randomization-based inference is especially important in experimental design and in survey sampling.

In fields such as epidemiology, social sciences, psychology and statistics, an observational study draws inferences from a sample to a population where the independent variable is not under the control of the researcher because of ethical concerns or logistical constraints. One common observational study is about the possible effect of a treatment on subjects, where the assignment of subjects into a treated group versus a control group is outside the control of the investigator. This is in contrast with experiments, such as randomized controlled trials, where each subject is randomly assigned to a treated group or a control group. Observational studies, for lacking an assignment mechanism, naturally present difficulties for inferential analysis.
Therapeutic misconception is a common ethical problem encountered in human subjects research. It was originally described in 1982 by Paul Appelbaum and colleagues. The idea was introduced to the bioethics community in 1987. The formulation given by Appelbaum et al. in 1987 was the following: “To maintain a therapeutic misconception is to deny the possibility that there may be major disadvantages to participating in clinical research that stem from the nature of the research process itself.”

Placebo-controlled studies are a way of testing a medical therapy in which, in addition to a group of subjects that receives the treatment to be evaluated, a separate control group receives a sham "placebo" treatment which is specifically designed to have no real effect. Placebos are most commonly used in blinded trials, where subjects do not know whether they are receiving real or placebo treatment. Often, there is also a further "natural history" group that does not receive any treatment at all.
A cluster-randomised controlled trial is a type of randomised controlled trial in which groups of subjects are randomised. Cluster randomised controlled trials are also known as cluster-randomised trials, group-randomised trials, and place-randomized trials. Cluster-randomised controlled trials are used when there is a strong reason for randomising treatment and control groups over randomising participants.

Gemigliptin (rINN), sold under the brand name Zemiglo, is an oral anti-hyperglycemic agent of the dipeptidyl peptidase-4 inhibitor class of drugs. Glucose lowering effects of DPP-4 inhibitors are mainly mediated by GLP-1 and gastric inhibitory polypeptide (GIP) incretin hormones which are inactivated by DPP-4.

ZMapp is an experimental biopharmaceutical drug comprising three chimeric monoclonal antibodies under development as a treatment for Ebola virus disease. Two of the three components were originally developed at the Public Health Agency of Canada's National Microbiology Laboratory (NML), and the third at the U.S. Army Medical Research Institute of Infectious Diseases; the cocktail was optimized by Gary Kobinger, a research scientist at the NML and underwent further development under license by Mapp Biopharmaceutical. ZMapp was first used on humans during the Western African Ebola virus epidemic, having only been previously tested on animals and not yet subjected to a randomized controlled trial. The National Institutes of Health (NIH) ran a clinical trial starting in January 2015 with subjects from Sierra Leone, Guinea, and Liberia aiming to enroll 200 people, but the epidemic waned and the trial closed early, leaving it too statistically underpowered to give a meaningful result about whether ZMapp worked.
Marvin Zelen was Professor Emeritus of Biostatistics in the Department of Biostatistics at the Harvard T.H. Chan School of Public Health (HSPH), and Lemuel Shattuck Research Professor of Statistical Science. During the 1980s, Zelen chaired HSPH's Department of Biostatistics. Among colleagues in the field of statistics, he was widely known as a leader who shaped the discipline of biostatistics. He "transformed clinical trial research into a statistically sophisticated branch of medical research."

The Randomised Evaluation of COVID-19 Therapy is a large-enrollment clinical trial of possible treatments for people in the United Kingdom admitted to hospital with severe COVID-19 infection. The trial was later expanded to Indonesia, Nepal and Vietnam. The trial has tested ten interventions on adults: eight repurposed drugs, one newly developed drug and convalescent plasma.
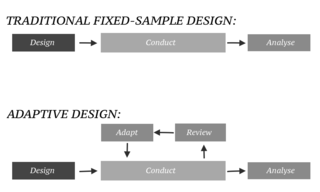
In an adaptive design of a clinical trial, the parameters and conduct of the trial for a candidate drug or vaccine may be changed based on an interim analysis. Adaptive design typically involves advanced statistics to interpret a clinical trial endpoint. This is in contrast to traditional single-arm clinical trials or randomized clinical trials (RCTs) that are static in their protocol and do not modify any parameters until the trial is completed. The adaptation process takes place at certain points in the trial, prescribed in the trial protocol. Importantly, this trial protocol is set before the trial begins with the adaptation schedule and processes specified. Adaptions may include modifications to: dosage, sample size, drug undergoing trial, patient selection criteria and/or "cocktail" mix. The PANDA provides not only a summary of different adaptive designs, but also comprehensive information on adaptive design planning, conduct, analysis and reporting.
References
- Zelen, Marvin (1979). "A New Design for Randomized Clinical Trials". The New England Journal of Medicine . 300 (22): 1242–1245. doi:10.1056/NEJM197905313002203. PMID 431682.
- Torgerson, D. J.; Roland, M. (1998). "What is Zelen's design?". BMJ. 316 (7131): 606. doi:10.1136/bmj.316.7131.606. PMC 1112637 . PMID 9518917.
- Palmer, C. R. (2002). "Ethics, data-dependent designs, and the strategy of clinical trials: time to start learning-as-we-go?". Statistical Methods in Medical Research. 11 (5): 381–402. CiteSeerX 10.1.1.128.9963 . doi:10.1191/0962280202sm298ra. ISSN 0962-2802. PMID 12357585. S2CID 1818466.