Related Research Articles

Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is acute if it resolves within six months, and chronic if it lasts longer than six months. Acute hepatitis can resolve on its own, progress to chronic hepatitis, or (rarely) result in acute liver failure. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer.

Jaundice, also known as icterus, is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary-tract obstruction. The prevalence of jaundice in adults is rare, while jaundice in babies is common, with an estimated 80% affected during their first week of life. The most commonly associated symptoms of jaundice are itchiness, pale feces, and dark urine.

Hepatitis C is an infectious disease caused by the hepatitis C virus (HCV) that primarily affects the liver; it is a type of viral hepatitis. During the initial infection period, people often have mild or no symptoms. Early symptoms can include fever, dark urine, abdominal pain, and yellow tinged skin. The virus persists in the liver, becoming chronic, in about 70% of those initially infected. Early on, chronic infection typically has no symptoms. Over many years however, it often leads to liver disease and occasionally cirrhosis. In some cases, those with cirrhosis will develop serious complications such as liver failure, liver cancer, or dilated blood vessels in the esophagus and stomach.
Liver function tests, also referred to as a hepatic panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin time (aPTT), albumin, bilirubin, and others. The liver transaminases aspartate transaminase and alanine transaminase are useful biomarkers of liver injury in a patient with some degree of intact liver function.
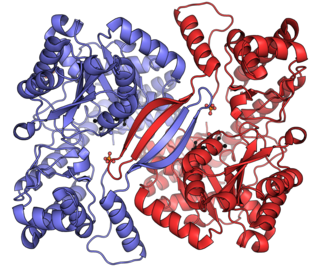
Alanine transaminase (ALT) is a transaminase enzyme. It is also called alanine aminotransferase and was formerly called serum glutamate-pyruvate transaminase or serum glutamic-pyruvic transaminase (SGPT) and was first characterized in the mid-1950s by Arthur Karmen and colleagues. ALT is found in plasma and in various body tissues but is most common in the liver. It catalyzes the two parts of the alanine cycle. Serum ALT level, serum AST level, and their ratio are routinely measured clinically as biomarkers for liver health.

Alcoholic liver disease (ALD), also called alcohol-related liver disease (ARLD), is a term that encompasses the liver manifestations of alcohol overconsumption, including fatty liver, alcoholic hepatitis, and chronic hepatitis with liver fibrosis or cirrhosis.

Hepatotoxicity implies chemical-driven liver damage. Drug-induced liver injury (DILI) is a cause of acute and chronic liver disease caused specifically by medications and the most common reason for a drug to be withdrawn from the market after approval.

Alcoholic hepatitis is hepatitis due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day. It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice, ascites, fatigue and hepatic encephalopathy. Mild cases are self-limiting, but severe cases have a high risk of death. Severity in alcoholic hepatitis is determined several clinical prediction models such as the Maddrey's Discriminant Function and the MELD score.

Autoimmune hepatitis, formerly known as lupoid hepatitis, plasma cell hepatitis, or autoimmune chronic active hepatitis, is a chronic, autoimmune disease of the liver that occurs when the body's immune system attacks liver cells, causing the liver to be inflamed. Common initial symptoms may include fatigue, nausea, muscle aches, or weight loss or signs of acute liver inflammation including fever, jaundice, and right upper quadrant abdominal pain. Individuals with autoimmune hepatitis often have no initial symptoms and the disease may be detected by abnormal liver function tests and increased protein levels during routine bloodwork or the observation of an abnormal-looking liver during abdominal surgery.

Liver disease, or hepatic disease, is any of many diseases of the liver. If long-lasting it is termed chronic liver disease. Although the diseases differ in detail, liver diseases often have features in common.

Fatty liver disease (FLD), also known as hepatic steatosis and steatotic liver disease (SLD), is a condition where excess fat builds up in the liver. Often there are no or few symptoms. Occasionally there may be tiredness or pain in the upper right side of the abdomen. Complications may include cirrhosis, liver cancer, and esophageal varices.

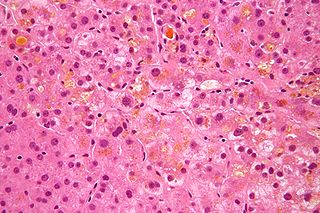
Liver biopsy is the biopsy from the liver. It is a medical test that is done to aid diagnosis of liver disease, to assess the severity of known liver disease, and to monitor the progress of treatment.
Cholestasis is a condition where the flow of bile from the liver to the duodenum is impaired. The two basic distinctions are:
Chronic liver disease in the clinical context is a disease process of the liver that involves a process of progressive destruction and regeneration of the liver parenchyma leading to fibrosis and cirrhosis. "Chronic liver disease" refers to disease of the liver which lasts over a period of six months. It consists of a wide range of liver pathologies which include inflammation, liver cirrhosis, and hepatocellular carcinoma. The entire spectrum need not be experienced.
In medicine, the presence of elevated transaminases, commonly the transaminases alanine transaminase (ALT) and aspartate transaminase (AST), may be an indicator of liver dysfunction. Other terms include transaminasemia, transaminitis, and elevatedliver enzymes. Normal ranges for both ALT and AST vary by gender, age, and geography and are roughly 8-40 U/L. Mild transaminesemia refers to levels up to 250 U/L. Drug-induced increases such as that found with the use of anti-tuberculosis agents such as isoniazid are limited typically to below 100 U/L for either ALT or AST. Muscle sources of the enzymes, such as intense exercise, are unrelated to liver function and can markedly increase AST and ALT. Cirrhosis of the liver or fulminant liver failure secondary to hepatitis commonly reach values for both ALT and AST in the >1000 U/L range; however, many people with liver disease have normal transaminases. Elevated transaminases that persist less than six months are termed "acute" in nature, and those values that persist for six months or more are termed "chronic" in nature.

Hepatitis B is an infectious disease caused by the Hepatitis B virus (HBV) that affects the liver; it is a type of viral hepatitis. It can cause both acute and chronic infection.

Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage to the liver leads to repair of liver tissue and subsequent formation of scar tissue. Over time, scar tissue can replace normal functioning tissue, leading to the impaired liver function of cirrhosis. The disease typically develops slowly over months or years. Early symptoms may include tiredness, weakness, loss of appetite, unexplained weight loss, nausea and vomiting, and discomfort in the right upper quadrant of the abdomen. As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin. The fluid build-up in the abdomen may develop into spontaneous infections. More serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus, stomach, or intestines, and liver cancer. Stages of cirrhosis include compensated cirrhosis and decompensated cirrhosis.
FibroTest, known as FibroSure in the US, is a biomarker test that uses the results of six blood serum tests to generate a score that is correlated with the degree of liver damage in people with a variety of liver diseases. FibroTest has the same prognostic value as a liver biopsy. FibroSure uses quantitative results of five serum biochemical markers, α2-macroglobulin, haptoglobin, apolipoprotein A1, bilirubin, gamma glutamyl transpeptidase (GGT), with a patient’s age and gender to generate a measure of fibrosis and necroinflammatory activity in the liver.
A liver support system or diachysis is a type of therapeutic device to assist in performing the functions of the liver. Such systems focus either on removing the accumulating toxins, or providing additional replacement of the metabolic functions of the liver through the inclusion of hepatocytes to the device. This system is in trial to help people with acute liver failure (ALF) or acute-on-chronic liver failure.
Hyperbilirubinemia is a clinical condition describing an elevation of blood bilirubin level due to the inability to properly metabolise or excrete bilirubin, a product of erythrocytes breakdown. In severe cases, it is manifested as jaundice, the yellowing of tissues like skin and the sclera when excess bilirubin deposits in them. The US records 52,500 jaundice patients annually. By definition, bilirubin concentration of greater than 3 mg/ml is considered hyperbilirubinemia, following which jaundice progressively develops and becomes apparent when plasma levels reach 20 mg/ml. Rather than a disease itself, hyperbilirubinemia is indicative of multifactorial underlying disorders that trace back to deviations from regular bilirubin metabolism. Diagnosis of hyperbilirubinemia depends on physical examination, urinalysis, serum tests, medical history and imaging to identify the cause. Genetic diseases, alcohol, pregnancy and hepatitis viruses affect the likelihood of hyperbilirubinemia. Causes of hyperbilirubinemia mainly arise from the liver. These include haemolytic anaemias, enzymatic disorders, liver damage and gallstones. Hyperbilirubinemia itself is often benign. Only in extreme cases does kernicterus, a type of brain injury, occur. Therapy for adult hyperbilirubinemia targets the underlying diseases but patients with jaundice often have poor outcomes.
References
- ↑ Nyblom H, Berggren U, Balldin J, Olsson R (2004). "High AST/ALT ratio may indicate advanced alcoholic liver disease rather than heavy drinking". Alcohol and Alcoholism. 39 (4): 336–9. doi: 10.1093/alcalc/agh074 . PMID 15208167.
- ↑ Nyblom H, Björnsson E, Simrén M, Aldenborg F, Almer S, Olsson R (September 2006). "The AST/ALT ratio as an indicator of cirrhosis in patients with PBC". Liver International. 26 (7): 840–5. doi:10.1111/j.1478-3231.2006.01304.x. PMID 16911467. S2CID 3126986.
- ↑ Gopal DV, Rosen HR (February 2000). "Abnormal findings on liver function tests. Interpreting results to narrow the diagnosis and establish a prognosis". Postgraduate Medicine. 107 (2): 100–2, 105–9, 113–4. doi:10.3810/pgm.2000.02.869. PMID 10689411. S2CID 30483587.[ permanent dead link ]
- ↑ Moussavian, S. N.; Becker, R. C.; Piepmeyer, J. L.; Mezey, E.; Bozian, R. C. (Mar 1985). "Serum gamma-glutamyl transpeptidase and chronic alcoholism. Influence of alcohol ingestion and liver disease". Digestive Diseases and Sciences. 30 (3): 211–4. doi:10.1007/bf01347885. PMID 2857631. S2CID 24588657.
- ↑ Giboney, Paul T. (2005-03-15). "Mildly Elevated Liver Transaminase Levels in the Asymptomatic Patient". American Family Physician. 71 (6): 1105–1110. ISSN 0002-838X. PMID 15791889.
- ↑ Pettersson, J.; et al. (2007). "Muscular exercise can cause highly pathological liver function tests in healthy men". British Journal of Clinical Pharmacology. 65 (2): 253–259. doi:10.1111/j.1365-2125.2007.03001.x. PMC 2291230 . PMID 17764474.
- ↑ Kenneth D. McClatchey (2002). Clinical laboratory medicine. Lippincott Williams & Wilkins. pp. 288–. ISBN 978-0-683-30751-1 . Retrieved 21 May 2010.
- 1 2 De Ritis F, Coltorti M, Giusti G (July 2006). "An enzymic test for the diagnosis of viral hepatitis: the transaminase serum activities. 1957". Clinica Chimica Acta. 369 (2): 148–52. doi:10.1016/j.cca.2006.05.001. PMID 16781697.
- ↑ Botros, Mona; Sikaris, Kenneth (November 2013). "The De Ritis Ratio: The Test of Time". The Clinical Biochemist. Reviews. 34 (3): 117–130. PMC 3866949 . PMID 24353357.
- ↑ Lazo, Mariana. "Liver Function". Johns Hopkins Medicine. Retrieved 7 July 2022.
- ↑ Botros, Mona; Sikaris, Kenneth (November 2013). "The De Ritis Ratio: The Test of Time". The Clinical Biochemist. Reviews. 34 (3): 117–130. PMC 3866949 . PMID 24353357.