Myelodysplastic syndromes (MDS) are a group of cancers in which immature blood cells in the bone marrow do not mature and therefore do not become healthy blood cells. Early on, there are typically no symptoms. Later symptoms may include feeling tired, shortness of breath, easy bleeding, or frequent infections. Some types may develop into acute myeloid leukemia.

Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys no longer function. It is divided into acute kidney failure and chronic kidney failure. Symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, or confusion. Complications of acute disease may include uremia, high blood potassium, or volume overload. Complications of chronic disease may include heart disease, high blood pressure, or anemia.

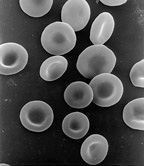
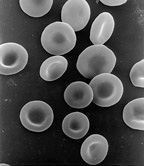
The hematocrit, also known by several other names, is the volume percentage (vol%) of red blood cells in blood. It is normally 47% ±5% for men and 42% ±5% for women. It is considered an integral part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count, and platelet count. Because the purpose of red blood cells is to transfer oxygen from the lungs to body tissues, a blood sample's hematocrit—the red blood cell volume percentage—can become a point of reference of its capability of delivering oxygen. The measure of a subject's hematocrit levels can indicate possible disease. An abnormally low hematocrit may suggest anemia, a decrease in the total amount of red blood cells, while an abnormally high hematocrit is called polycythemia. Both are potentially life-threatening disorders.

Uremia is the condition of having high levels of urea in the blood. Urea is one of the primary components of urine. It can be defined as an excess of amino acid and protein metabolism end products, such as urea and creatinine, in the blood that would be normally excreted in the urine. Uremic syndrome can be defined as the terminal clinical manifestation of kidney failure. It is the signs, symptoms and results from laboratory tests which result from inadequate excretory, regulatory and endocrine function of the kidneys. Both uremia and uremic syndrome have been used interchangeably to denote a very high plasma urea concentration that is the result of renal failure. The former denotation will be used for the rest of the article.

Ischemia or ischaemia is a restriction in blood supply to tissues, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue. It also means local anemia in a given part of a body sometimes resulting from constriction. Ischemia comprises not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total.
Hematemesis is the vomiting of blood. The source is generally the upper gastrointestinal tract, typically above the suspensory muscle of duodenum. Patients can easily confuse it with hemoptysis, although the latter is more common. Hematemesis "is always an important sign".
Iron-deficiency anemia is anemia caused by a lack of iron. Anemia is defined as a decrease in the number of red blood cells or the amount of hemoglobin in the blood. When onset is slow, symptoms are often vague such as feeling tired, weak, short of breath, or having decreased ability to exercise. Anemia that comes on quickly often has more severe symptoms, including: confusion, feeling like one is going to pass out or increased thirst. Anemia is typically significant before a person becomes noticeably pale. Children with iron deficiency anemia may have problems with growth and development. There may be additional symptoms depending on the underlying cause.
The mean corpuscular volume, or mean cell volume (MCV), is a measure of the average volume of a red blood corpuscle. The measure is attained by multiplying a volume of blood by the proportion of blood that is cellular, and dividing that product by the number of erythrocytes in that volume. The mean corpuscular volume is a part of a standard complete blood count.
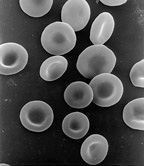
Red blood cell distribution width is a measure of the range of variation of red blood cell (RBC) volume that is reported as part of a standard complete blood count. Usually red blood cells are a standard size of about 6-8 μm in diameter. Certain disorders, however, cause a significant variation in cell size. Higher RDW values indicate greater variation in size. Normal reference range of RDW-CV in human red blood cells is 11.5-14.5%. If anemia is observed, RDW test results are often used together with mean corpuscular volume (MCV) results to determine the possible causes of the anemia. It is mainly used to differentiate an anemia of mixed causes from an anemia of a single cause.

Pallor is a pale color of the skin that can be caused by illness, emotional shock or stress, stimulant use, or anemia, and is the result of a reduced amount of oxyhaemoglobin and is visible in skin conjuctivae or mucous membrane.

Megaloblastic anemia is an anemia that results from inhibition of DNA synthesis during red blood cell production. When DNA synthesis is impaired, the cell cycle cannot progress from the G2 growth stage to the mitosis (M) stage. This leads to continuing cell growth without division, which presents as macrocytosis. Megaloblastic anemia has a rather slow onset, especially when compared to that of other anemias. The defect in red cell DNA synthesis is most often due to hypovitaminosis, specifically vitamin B12 deficiency or folate deficiency. Loss of micronutrients may also be a cause. Copper deficiency resulting from an excess of zinc from unusually high oral consumption of zinc-containing denture-fixation creams has been found to be a cause.
An exchange transfusion is a blood transfusion in which the patient's blood or components of it are exchanged with other blood or blood products. The patient's blood is removed and replaced by donated blood or blood components. This exchange transfusion can be performed manually or using a machine (apheresis).
The term macrocytic is from Greek words meaning "large cell". A macrocytic class of anemia is an anemia in which the red blood cells (erythrocytes) are larger than their normal volume. The normal erythrocyte volume in humans is about 80 to 100 femtoliters. In metric terms the size is given in equivalent cubic micrometers. The condition of having erythrocytes which are too large, is called macrocytosis. In contrast, in microcytic anemia, the erythrocytes are smaller than normal.
Hematologic diseases are disorders which primarily affect the blood. Hematology includes the study of these disorders.

Stomach diseases include gastritis, gastroparesis, diarrhea, Crohn's disease and various cancers.
Patient Blood Management (PBM) is a multidisciplinary, evidence-based approach to optimizing the care of patients who might need a blood transfusion. Patient blood management represents an international initiative in best practice for transfusion medicine that is supported by the World Health Organization (WHO). Establishing a patient blood management strategy requires leadership and support from national and regional government policymakers and managers, healthcare professionals, and patients. Patients are an essential part of planning, implementing and evaluating PBM programs. Examples of how to implement PBM are available from Australia, the UK, and the USA.
Drug-induced autoimmune hemolytic anemia is a form of hemolytic anemia.
A Cameron lesion is a linear erosion or ulceration of the mucosal folds lining the stomach where it is constricted by the thoracic diaphragm in persons with large hiatal hernias. The lesions may cause chronic blood loss resulting in iron deficiency anemia; less often they cause acute bleeding.