The United States Food and Drug Administration is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food safety, tobacco products, dietary supplements, prescription and over-the-counter pharmaceutical drugs (medications), vaccines, biopharmaceuticals, blood transfusions, medical devices, electromagnetic radiation emitting devices (ERED), cosmetics, animal foods & feed and veterinary products.

Current Good manufacturing practices (cGMP) are those conforming to the guidelines recommended by relevant agencies. Those agencies control the authorization and licensing of the manufacture and sale of food and beverages, cosmetics, pharmaceutical products, dietary supplements, and medical devices. These guidelines provide minimum requirements that a manufacturer must meet to assure that their products are consistently high in quality, from batch to batch, for their intended use. The rules that govern each industry may differ significantly; however, the main purpose of GMP is always to prevent harm from occurring to the end user. Additional tenets include ensuring the end product is free from contamination, that it is consistent in its manufacture, that its manufacture has been well documented, that personnel are well trained, and that the product has been checked for quality more than just at the end phase. GMP is typically ensured through the effective use of a quality management system (QMS).
Pharmacovigilance, also known as drug safety, is the pharmaceutical science relating to the "collection, detection, assessment, monitoring, and prevention" of adverse effects with pharmaceutical products. The etymological roots for the word "pharmacovigilance" are: pharmakon and vigilare. As such, pharmacovigilance heavily focuses on adverse drug reactions (ADR), which are defined as any response to a drug which is noxious and unintended, including lack of efficacy. Medication errors such as overdose, and misuse and abuse of a drug as well as drug exposure during pregnancy and breastfeeding, are also of interest, even without an adverse event, because they may result in an adverse drug reaction.

The United States Federal Food, Drug, and Cosmetic Act is a set of laws passed by the United States Congress in 1938 giving authority to the U.S. Food and Drug Administration (FDA) to oversee the safety of food, drugs, medical devices, and cosmetics. A principal author of this law was Royal S. Copeland, a three-term U.S. senator from New York. In 1968, the Electronic Product Radiation Control provisions were added to the FD&C. Also in that year the FDA formed the Drug Efficacy Study Implementation (DESI) to incorporate into FD&C regulations the recommendations from a National Academy of Sciences investigation of effectiveness of previously marketed drugs. The act has been amended many times, most recently to add requirements about bioterrorism preparations.
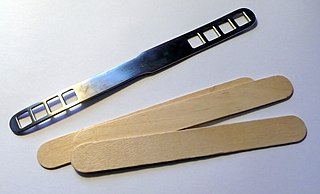
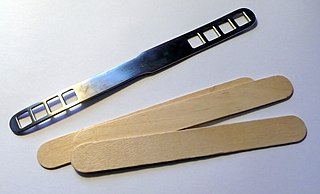
A medical device is any device intended to be used for medical purposes. Significant potential for hazards are inherent when using a device for medical purposes and thus medical devices must be proved safe and effective with reasonable assurance before regulating governments allow marketing of the device in their country. As a general rule, as the associated risk of the device increases the amount of testing required to establish safety and efficacy also increases. Further, as associated risk increases the potential benefit to the patient must also increase.
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. The term complication is similar to adverse effect, but the latter is typically used in pharmacological contexts, or when the negative effect is expected or common. If the negative effect results from an unsuitable or incorrect dosage or procedure, this is called a medical error and not an adverse effect. Adverse effects are sometimes referred to as "iatrogenic" because they are generated by a physician/treatment. Some adverse effects occur only when starting, increasing or discontinuing a treatment. Adverse effects can also be caused by placebo treatments . Using a drug or other medical intervention which is contraindicated may increase the risk of adverse effects. Adverse effects may cause complications of a disease or procedure and negatively affect its prognosis. They may also lead to non-compliance with a treatment regimen. Adverse effects of medical treatment resulted in 142,000 deaths in 2013 up from 94,000 deaths in 1990 globally.
An adverse event (AE) is any untoward medical occurrence in a patient or clinical investigation subject administered a pharmaceutical product and which does not necessarily have a causal relationship with this treatment. An adverse event can therefore be any unfavourable and unintended sign, symptom, or disease temporally associated with the use of a medicinal (investigational) product, whether or not related to the medicinal (investigational) product.
A drug recall removes a prescription or over-the-counter drug from the market. Drug recalls in the United States are made by the FDA or the creators of the drug when certain criteria are met. When a drug recall is made, the drug is removed from the market and potential legal action can be taken depending on the severity of the drug recall.
Postmarketing surveillance (PMS), also known as post market surveillance, is the practice of monitoring the safety of a pharmaceutical drug or medical device after it has been released on the market and is an important part of the science of pharmacovigilance. Since drugs and medical devices are approved on the basis of clinical trials, which involve relatively small numbers of people who have been selected for this purpose – meaning that they normally do not have other medical conditions which may exist in the general population – postmarketing surveillance can further refine, or confirm or deny, the safety of a drug or device after it is used in the general population by large numbers of people who have a wide variety of medical conditions.

The Center for Devices and Radiological Health (CDRH) is the branch of the United States Food and Drug Administration (FDA) responsible for the premarket approval of all medical devices, as well as overseeing the manufacturing, performance and safety of these devices. The CDRH also oversees the radiation safety performance of non-medical devices which emit certain types of electromagnetic radiation, such as cellular phones and microwave ovens.

MedWatch is the Food and Drug Administration’s “Safety Information and Adverse Event Reporting Program.” It interacts with the FDA Adverse Event Reporting System. MedWatch is used for reporting an adverse event or sentinel event. Founded in 1993, this system of voluntary reporting allows such information to be shared with the medical community or the general public. The system includes publicly available databases and online analysis tools for professionals. MedWatch also distributes information on medical recalls and other clinical safety communications via its platforms.

President of the United States George W. Bush signed the Food and Drug Administration Amendments Act of 2007 (FDAAA) on September 27, 2007. This law reviewed, expanded, and reaffirmed several existing pieces of legislation regulating the FDA. These changes allow the FDA to perform more comprehensive reviews of potential new drugs and devices. It was sponsored by Reps. Joe Barton and Frank Pallone and passed unanimously by the Senate.
Design controls designates the application of a formal methodology to the conduct of product development activities. It is often mandatory to implement such practice when designing and developing products within regulated industries.
The following outline is provided as an overview of and topical guide to clinical research:
The Unique Device Identification (UDI) System is intended to assign a unique identifier to medical devices within the United States, Europe, China, South Korea, Saudi Arabia and Taiwan. It was signed into law in the US on September 27, 2007, as part of the Food and Drug Administration Amendments Act of 2007.

The United States Food and Drug Administration Modernization Act of 1997 (FDAMA) amended the Federal Food, Drug, and Cosmetic Act. This act is related to the regulation of food, drugs, devices, and biological products by the FDA. These changes were made in order to recognize the changes in the way the FDA would be operating in the 21st century. The main focus of this is the acknowledgment in the advancement of technological, trade, and public health complexities.

The Food and Drug Administration Safety and Innovation Act of 2012 (FDASIA) is a piece of American regulatory legislation signed into law on July 9, 2012. It gives the United States Food and Drug Administration (FDA) the authority to collect user fees from the medical industry to fund reviews of innovator drugs, medical devices, generic drugs and biosimilar biologics. It also creates the breakthrough therapy designation program and extends the priority review voucher program to make eligible rare pediatric diseases. The measure was passed by 96 senators voting for and one voting against.

Safe Medical Device Amendments of 1990 or Safe Medical Devices Act sanctioned progressive reporting and tracking rules for medical devices classified by the Medical Device Regulation Act. The Act mandates reporting requirements by medical device manufacturers regarding adverse safety events and product effectiveness of devices classified as substantially equivalent to Class III medical devices. The United States Statute established the Health and Human Services Office of International Relations and a U.S. Food and Drug Administration office for regulatory activities concerning healthcare products which are considered a combinational biological, device, or drug product. The Act of Congress transferred the electronic product radiation control provisions established by the Radiation Control for Health and Safety Act.
Single-use medical device reprocessing is the disinfection, cleaning, remanufacturing, testing, packaging and labeling, and sterilization among other steps, of a used,, medical device to be put in service again. All reprocessed medical devices originally labeled for single use in the United States are subject to U.S. Food and Drug Administration (FDA) manufacturing requirements and must meet strict cleaning, functionality, and sterility specifications prior to use. Although first regulated in the U.S., the reprocessing of medical devices, particularly those that are labeled "Single Use Device" (SUDs), is a global practice with countries in Europe, Asia, Africa, and North America actively engaged in reprocessing. Currently, approximately 2% of all SUDs on the U.S. market are eligible for reprocessing by a qualified commercial vendor. Reprocessing industry estimates indicate the amount of revenue saved by hospitals that use reprocessed devices to be $471 million in 2018. Over 8,800 hospitals and surgical centers use reprocessed devices, in the U.S., Canada, Israel, Europe and Japan, according to the Association of Medical Device Reprocessors.

The Drug Quality and Security Act is a law that amended the Federal Food, Drug, and Cosmetic Act to grant the Food and Drug Administration more authority to regulate and monitor the manufacturing of compounded drugs. The bill was written in response to the New England Compounding Center meningitis outbreak that took place in 2012, which killed 64 people. The bill was signed by President Obama on November 27, 2013.