Related Research Articles
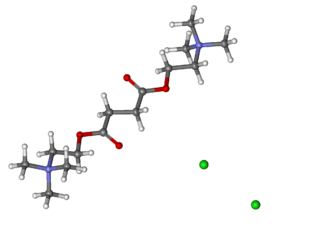
Suxamethonium chloride, also known as suxamethonium or succinylcholine, or simply sux by medical abbreviation, is a medication used to cause short-term paralysis as part of general anesthesia. This is done to help with tracheal intubation or electroconvulsive therapy. It is administered by injection, either into a vein or into a muscle. When used in a vein, onset of action is generally within one minute and effects last for up to 10 minutes.

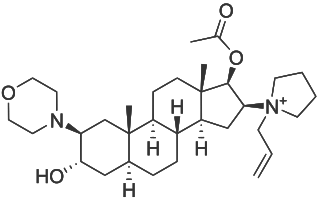
Pancuronium is an aminosteroid muscle relaxant with various medical uses. It is used in euthanasia and is used in some states as the second of three drugs administered during lethal injections in the United States.
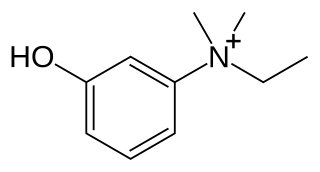
Edrophonium is a readily reversible acetylcholinesterase inhibitor. It prevents breakdown of the neurotransmitter acetylcholine and acts by competitively inhibiting the enzyme acetylcholinesterase, mainly at the neuromuscular junction. It is sold under the trade names Tensilon and Enlon.
Neostigmine, sold under the brand name Bloxiverz, among others, is a medication used to treat myasthenia gravis, Ogilvie syndrome, and urinary retention without the presence of a blockage. It is also used in anaesthesia to end the effects of non-depolarising neuromuscular blocking medication. It is given by injection either into a vein, muscle, or under the skin. After injection effects are generally greatest within 30 minutes and last up to 4 hours.

Pyridostigmine is a medication used to treat myasthenia gravis and underactive bladder. It is also used together with atropine to end the effects of neuromuscular blocking medication of the non-depolarizing type. It is typically given by mouth but can also be used by injection. The effects generally begin within 45 minutes and last up to 6 hours.

Vecuronium bromide, sold under the brand name Norcuron among others, is a medication used as part of general anesthesia to provide skeletal muscle relaxation during surgery or mechanical ventilation. It is also used to help with endotracheal intubation; however, agents such as suxamethonium (succinylcholine) or rocuronium are generally preferred if this needs to be done quickly. It is given by injection into a vein. Effects are greatest at about 4 minutes and last for up to an hour.
In advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.

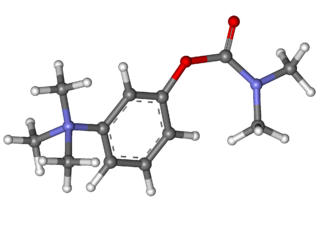
Glycopyrronium bromide is a medication of the muscarinic anticholinergic group. It does not cross the blood–brain barrier and consequently has few to no central effects. It is given by mouth, via intravenous injection, on the skin, and via inhalation. It is a synthetic quaternary ammonium compound. The cation, which is the active moiety, is called glycopyrronium (INN) or glycopyrrolate (USAN).

Neuromuscular-blocking drugs block neuromuscular transmission at the neuromuscular junction, causing paralysis of the affected skeletal muscles. This is accomplished via their action on the post-synaptic acetylcholine (Nm) receptors.
Rocuronium bromide is an aminosteroid non-depolarizing neuromuscular blocker or muscle relaxant used in modern anaesthesia to facilitate tracheal intubation by providing skeletal muscle relaxation, most commonly required for surgery or mechanical ventilation. It is used for standard endotracheal intubation, as well as for rapid sequence induction (RSI).

Rapacuronium bromide is a rapidly acting, non-depolarizing aminosteroid neuromuscular blocker formerly used in modern anaesthesia, to aid and enable endotracheal intubation, which is often necessary to assist in the controlled ventilation of unconscious patients during surgery and sometimes in intensive care. As a non-depolarizing agent it did not cause initial stimulation of muscles before weakening them.

Atracurium besilate, also known as atracurium besylate, is a medication used in addition to other medications to provide skeletal muscle relaxation during surgery or mechanical ventilation. It can also be used to help with endotracheal intubation but suxamethonium (succinylcholine) is generally preferred if this needs to be done quickly. It is given by injection into a vein. Effects are greatest at about 4 minutes and last for up to an hour.

Mivacurium chloride is a short-duration non-depolarizing neuromuscular-blocking drug or skeletal muscle relaxant in the category of non-depolarizing neuromuscular-blocking drugs, used adjunctively in anesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation.

Sugammadex, sold under the brand name Bridion, is a medication for the reversal of neuromuscular blockade induced by rocuronium and vecuronium in general anaesthesia. It is the first selective relaxant binding agent (SRBA). It is marketed by Merck.

Doxacurium chloride is a neuromuscular-blocking drug or skeletal muscle relaxant in the category of non-depolarizing neuromuscular-blocking drugs, used adjunctively in anesthesia to provide skeletal muscle relaxation during surgery or mechanical ventilation. Unlike a number of other related skeletal muscle relaxants, it is rarely used adjunctively to facilitate endotracheal intubation.

Alcuronium chloride is a neuromuscular blocking (NMB) agent, alternatively referred to as a skeletal muscle relaxant. It is a semi-synthetic substance prepared from C-toxiferine I, a bis-quaternary alkaloid obtained from Strychnos toxifera. C-toxiferine I itself has been tested for its pharmacological action and noted to be a very long acting neuromuscular blocking agent For a formal definition of the durations of actions associated with NMB agents, see page for gantacurium. The replacement of both the N-methyl groups with N-allyl moieties yielded N,N-diallyl-bis-nortoxiferine, now recognized as alcuronium.

Bambuterol (INN) is a long-acting β adrenoceptor agonist (LABA) used in the treatment of asthma; it also is a prodrug of terbutaline. Commercially, the AstraZeneca pharmaceutical company produces and markets bambuterol as Bambec and Oxeol.

Candocuronium iodide is an aminosteroid neuromuscular-blocking drug. Its use in anesthesia for endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation was briefly evaluated in clinical studies in India. However, further development was discontinued due to attendant cardiovascular effects, primarily tachycardia that was about the same as the clinically established pancuronium bromide. Candocuronium demonstrated a short duration in the body, but a rapid onset of action. It had little to no ganglion blocking activity, with a greater potency than pancuronium.

Postoperative residual curarization (PORC) or residual neuromuscular blockade (RNMB) is a residual paresis after emergence from general anesthesia that may occur with the use of neuromuscular-blocking drugs. Today residual neuromuscular blockade is defined as a train of four ratio of less than 0.9 when measuring the response to ulnar nerve stimulation at the adductor pollicis muscle using mechanomyography or electromyography. A meta-analysis reported that the incidence of residual neuromuscular paralysis was 41% in patients receiving intermediate neuromuscular blocking agents during anaesthesia. It is possible that > 100,000 patients annually in the USA alone, are at risk of adverse events associated with undetected residual neuromuscular blockade. Neuromuscular function monitoring and the use of the appropriate dosage of sugammadex to reverse blockade produced by rocuronium can reduce the incidence of postoperative residual curarization. In this study, with usual care group receiving reversal with neostigmine resulted in a residual blockade rate of 43%.
Neuromuscular blocking agents, or in abbreviation, NMBAs, are chemical agents that paralyse skeletal muscles by blocking the movement of neurotransmitter at the neuromuscular junction. They are often used during general anesthesia to optimize intubating and surgical conditions, specifically to facilitate endotracheal intubation. This class of medications helps to reduce patient movement, breathing, or ventilator dyssynchrony and allows lower insufflation pressures during laparoscopy including the generation of nerve impulses. It has several indications for use in the intense care unit. It can help reduce hoarseness in voice as well as injury to the vocal cord during intubation. In addition, it plays an important role in facilitating mechanical ventilation in patients with poor lung function. In the following section, neuromuscular blocking agent's history, usages, mechanisms, side effects, interactions and pharmacology will further be elaborated and discussed.
References
- 1 2 "Glycopyrronium Bromide and Neostigmine Metilsulfate 0.5mg/2.5mg per ml Solution for Injection - Summary of Product Characteristics (SmPC)". (emc). 12 November 2018. Archived from the original on 7 August 2022. Retrieved 25 February 2023.
- 1 2 3 "Archived copy" (PDF). Archived (PDF) from the original on 26 February 2023. Retrieved 25 February 2023.
{{cite web}}: CS1 maint: archived copy as title (link) - 1 2 https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2023/216903Orig1s000ltr.pdf Archived 26 February 2023 at the Wayback Machine
 This article incorporates text from this source, which is in the public domain .
This article incorporates text from this source, which is in the public domain .