The substantia nigra (SN) is a basal ganglia structure located in the midbrain that plays an important role in reward and movement. Substantia nigra is Latin for "black substance", reflecting the fact that parts of the substantia nigra appear darker than neighboring areas due to high levels of neuromelanin in dopaminergic neurons. Parkinson's disease is characterized by the loss of dopaminergic neurons in the substantia nigra pars compacta.
Alpha-synuclein(aSyn) is a protein that, in humans, is encoded by the SNCA gene. Alpha-synuclein is a neuronal protein that regulates synaptic vesicle trafficking and subsequent neurotransmitter release.

Multiple system atrophy (MSA) is a rare neurodegenerative disorder characterized by autonomic dysfunction, tremors, slow movement, muscle rigidity, and postural instability and ataxia. This is caused by progressive degeneration of neurons in several parts of the brain including the basal ganglia, inferior olivary nucleus, and cerebellum.
Functional gastrointestinal disorders (FGID), also known as disorders of gut–brain interaction, include a number of separate idiopathic disorders which affect different parts of the gastrointestinal tract and involve visceral hypersensitivity and motility disturbances.
A neurodegenerative disease is caused by the progressive loss of structure or function of neurons, in the process known as neurodegeneration. Such neuronal damage may ultimately involve cell death. Neurodegenerative diseases include amyotrophic lateral sclerosis, multiple sclerosis, Parkinson's disease, Alzheimer's disease, Huntington's disease, multiple system atrophy, tauopathies, and prion diseases. Neurodegeneration can be found in the brain at many different levels of neuronal circuitry, ranging from molecular to systemic. Because there is no known way to reverse the progressive degeneration of neurons, these diseases are considered to be incurable; however research has shown that the two major contributing factors to neurodegeneration are oxidative stress and inflammation. Biomedical research has revealed many similarities between these diseases at the subcellular level, including atypical protein assemblies and induced cell death. These similarities suggest that therapeutic advances against one neurodegenerative disease might ameliorate other diseases as well.
In the management of Parkinson's disease, due to the chronic nature of Parkinson's disease (PD), a broad-based program is needed that includes patient and family education, support-group services, general wellness maintenance, exercise, and nutrition. At present, no cure for the disease is known, but medications or surgery can provide relief from the symptoms.
Dysbiosis is characterized by a disruption to the microbiome resulting in an imbalance in the microbiota, changes in their functional composition and metabolic activities, or a shift in their local distribution. For example, a part of the human microbiota such as the skin flora, gut flora, or vaginal flora, can become deranged, with normally dominating species underrepresented and normally outcompeted or contained species increasing to fill the void. Similar to the human gut microbiome, diverse microbes colonize the plant rhizosphere, and dysbiosis in the rhizosphere, can negatively impact plant health. Dysbiosis is most commonly reported as a condition in the gastrointestinal tract or plant rhizosphere.

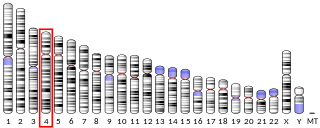
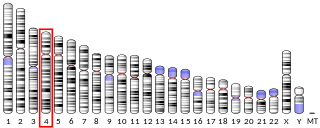
Leucine-rich repeat kinase 2 (LRRK2), also known as dardarin and PARK8, is a large, multifunctional kinase enzyme that in humans is encoded by the LRRK2 gene. LRRK2 is a member of the leucine-rich repeat kinase family. Variants of this gene are associated with an increased risk of Parkinson's disease and Crohn's disease.

Vacuolar protein sorting ortholog 35 (VPS35) is a protein involved in autophagy and is implicated in neurodegenerative diseases, such as Parkinson's disease (PD) and Alzheimer's disease (AD). VPS35 is part of a complex called the retromer, which is responsible for transporting select cargo proteins between vesicular structures and the Golgi apparatus. Mutations in the VPS35 gene (VPS35) cause aberrant autophagy, where cargo proteins fail to be transported and dysfunctional or unnecessary proteins fail to be degraded. There are numerous pathways affected by altered VPS35 levels and activity, which have clinical significance in neurodegeneration. There is therapeutic relevance for VPS35, as interventions aimed at correcting VPS35 function are in speculation.

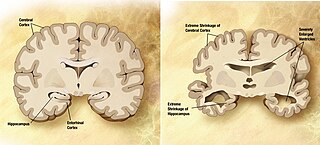
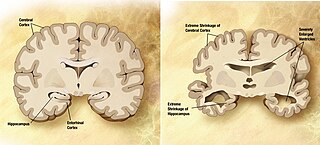
Parkinson's disease (PD), or simply Parkinson's, is a chronic degenerative disorder of the central nervous system that affects both the motor system and non-motor systems. The symptoms usually emerge slowly, and as the disease progresses, non-motor symptoms become more common. Early symptoms are tremor, rigidity, slowness of movement, and difficulty with walking. Problems may also arise with cognition, behaviour, sleep, and sensory systems. Parkinson's disease dementia is common in advanced stages.
Signs and symptoms of Parkinson's disease are varied. Parkinson's disease affects movement, producing motor symptoms. Non-motor symptoms, which include dysautonomia, cognitive and neurobehavioral problems, and sensory and sleep difficulties, are also common. When other diseases mimic Parkinson's disease, they are categorized as parkinsonism.
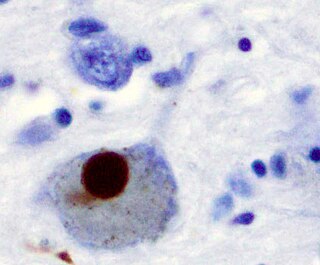
Parkinson's disease (PD) is a complicated neurodegenerative disease that progresses over time and is marked by bradykinesia, tremor, and stiffness. As the condition worsens, some patients may also experience postural instability. Parkinson's disease (PD) is primarily caused by the gradual degeneration of dopaminergic neurons in the region known as the substantia nigra along with other monoaminergic cell groups throughout the brainstem, increased activation of microglia, and the build-up of Lewy bodies and Lewy neurites, which are proteins found in surviving dopaminergic neurons.
Gene therapy in Parkinson's disease consists of the creation of new cells that produce a specific neurotransmitter (dopamine), protect the neural system, or the modification of genes that are related to the disease. Then these cells are transplanted to a patient with the disease. There are different kinds of treatments that focus on reducing the symptoms of the disease but currently there is no cure.

The gut–brain axis is the two-way biochemical signaling that takes place between the gastrointestinal tract and the central nervous system (CNS). The "microbiota–gut–brain axis" includes the role of gut microbiota in the biochemical signaling events that take place between the GI tract and the CNS. Broadly defined, the gut–brain axis includes the central nervous system, neuroendocrine system, neuroimmune systems, the hypothalamic–pituitary–adrenal axis, sympathetic and parasympathetic arms of the autonomic nervous system, the enteric nervous system, vagus nerve, and the gut microbiota.
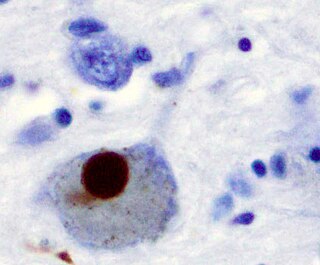
Synucleinopathies are neurodegenerative diseases characterised by the abnormal accumulation of aggregates of alpha-synuclein protein in neurons, nerve fibres or glial cells. There are three main types of synucleinopathy: Parkinson's disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA). Other rare disorders, such as various neuroaxonal dystrophies, also have α-synuclein pathologies. Additionally, autopsy studies have shown that around 6% of sporadic Alzheimer's Disease exhibit α-synuclein positive Lewy pathology, and are sub-classed as Alzheimer's Disease with Amygdalar Restricted Lewy Bodies (AD/ALB).

Neurodegenerative diseases are a heterogeneous group of complex disorders linked by the degeneration of neurons in either the peripheral nervous system or the central nervous system. Their underlying causes are extremely variable and complicated by various genetic and/or environmental factors. These diseases cause progressive deterioration of the neuron resulting in decreased signal transduction and in some cases even neuronal death. Peripheral nervous system diseases may be further categorized by the type of nerve cell affected by the disorder. Effective treatment of these diseases is often prevented by lack of understanding of the underlying molecular and genetic pathology. Epigenetic therapy is being investigated as a method of correcting the expression levels of misregulated genes in neurodegenerative diseases.

The pathophysiology of Parkinson's disease is death of dopaminergic neurons as a result of changes in biological activity in the brain with respect to Parkinson's disease (PD). There are several proposed mechanisms for neuronal death in PD; however, not all of them are well understood. Five proposed major mechanisms for neuronal death in Parkinson's Disease include protein aggregation in Lewy bodies, disruption of autophagy, changes in cell metabolism or mitochondrial function, neuroinflammation, and blood–brain barrier (BBB) breakdown resulting in vascular leakiness.

Animal models of Parkinson's disease are essential in the research field and widely used to study Parkinson's disease. Parkinson's disease is a neurodegenerative disorder, characterized by the loss of dopaminergic neurons in the substantia nigra pars compacta (SNpc). The loss of the dopamine neurons in the brain, results in motor dysfunction, ultimately causing the four cardinal symptoms of PD: tremor, rigidity, postural instability, and bradykinesia. It is the second most prevalent neurodegenerative disease, following Alzheimer's disease. It is estimated that nearly one million people could be living with PD in the United States.
Rapid eye movement sleep behaviour disorder and Parkinson's disease is rapid eye movement sleep behavior disorder (RBD) that is associated with Parkinson's disease. RBC is linked genetically and neuropathologically to α- synuclein, a presynaptic neuronal protein that exerts deleterious effects on neighbouring proteins, leading to neuronal death. This pathology is linked to numerous other neurodegenerative disorders, such as Lewy bodies dementia, and collectively these disorders are known as synucleinopathies. Numerous reports over the past few years have stated the frequent association of synucleinopathies with REM sleep behaviour disorder (RBD). In particular, the frequent association of RBD with Parkinson's. In the general population the incidence of RBD is around 0.5%, compared to the prevalence of RBD in PD patients, which has been reported to be between 38% and 60%. The diagnosis and symptom onset of RBD typically precedes the onset of motor or cognitive symptoms of PD by a number of years, typically ranging anywhere from 2 to 15 years prior. Hence, this link could provide an important window of opportunity in the implementation of therapies and treatments, that could prevent or slow the onset of PD.

Epidemiological studies have shown lower age-related prevalence of Parkinson's disease in South Asians, with the rate of prevalence being around 52.7 per 100,000 as compared to a higher prevalence rate observed in populations with European origin, 108-257 per 100,000. Additionally, several studies have seen a higher prevalence of in women which contrasts with global data that observes a overall higher prevalence seen in men. Compared to most of the rest of the world, the South Asian countries seem to be on the lower end of PD prevalence. However, this is not to say that PD is not of concern in these countries. Over the past couple of years, the rate of Parkinson's has gone up in South Asia meaning that it is of high importance to study this pathological disease in these populations.