The periodontal ligament, commonly abbreviated as the PDL, is a group of specialized connective tissue fibers that essentially attach a tooth to the alveolar bone within which it sits. It inserts into root cementum one side and onto alveolar bone on the other.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A person who practices this specialty is known as a periodontist.
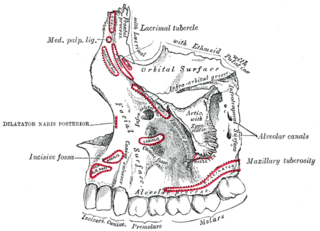
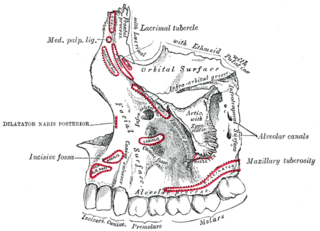
The alveolar process is the thickened ridge of bone that contains the tooth sockets on the jaw bones that hold teeth. In humans, the tooth-bearing bones are the maxilla and the mandible. The curved part of each alveolar process on the jaw is called the alveolar arch.

Edentulism or toothlessness is the condition of being toothless to at least some degree; in organisms that naturally have teeth (dentition), it is the result of tooth loss. Loss of some teeth is called partial edentulism, whereas loss of all teeth is called complete edentulism. Persons who have lost teeth are edentulous (edentate), whereas those who have not lost teeth can be called dentate by comparison. For example, a scientific study may include a partially edentulous group and a healthy dentate control group.

Maxillary sinus floor augmentation is a surgical procedure which aims to increase the amount of bone in the posterior maxilla, in the area of the premolar and molar teeth, by lifting the lower Schneiderian membrane and placing a bone graft.

A gingival graft, also called gum graft or periodontal plastic surgery, is a generic name for any of a number of periodontal surgical procedures in which the gum tissue is grafted. The aim may be to cover exposed root surfaces or merely to augment the band of keratinized tissue.

Crown lengthening is a surgical procedure performed by a dentist, or more frequently a specialist periodontist. There are a number of reasons for considering crown lengthening in a treatment plan. Commonly, the procedure is used to expose a greater amount of tooth structure for the purpose of subsequently restoring the tooth prosthetically. However, other indications include accessing subgingival caries, accessing perforations and to treat aesthetic disproportions such as a gummy smile. There are a number of procedures used to achieve an increase in crown length.
In dentistry, enamel matrix derivative (EMD) is an extract of porcine fetal tooth material used to biomimetically stimulate the soft and hard tissues surrounding teeth to regrow following tissue destruction.

In dentistry, a furcation defect is bone loss, usually a result of periodontal disease, affecting the base of the root trunk of a tooth where two or more roots meet. The extent and configuration of the defect are factors in both diagnosis and treatment planning.
Socket preservation or alveolar ridge preservation (ARP) is a procedure to reduce bone loss after tooth extraction to preserve the dental alveolus in the alveolar bone. A platelet rich fibrin (PRF) membrane containing bone growth enhancing elements is placed in the wound or a bone grafting material or scaffold is placed in the socket of an extracted tooth at the time of extraction. The socket is then directly closed with stitches or covered with a non-resorbable or resorbable membrane and sutured. After extraction, jaw bone has to be preserved to keep the socket in its original shape. Without socket preservation, the bone quickly resorbs resulting in 30–60% loss in bone volume in the six months after dental extraction. The jaw bone will never revert to its original shape once bone is lost and tissue contour has changed.

Peri-implantitis is a destructive inflammatory process affecting the soft and hard tissues surrounding dental implants. The soft tissues become inflamed whereas the alveolar bone, which surrounds the implant for the purposes of retention, is lost overtime. The bone loss involved in peri-implantitis differentiates this condition from peri-mucositis, a reversible inflammatory reaction involving only the soft tissues around the implant.
In dentistry, numerous types of classification schemes have been developed to describe the teeth and gum tissue in a way that categorizes various defects. All of these classification schemes combine to provide the periodontal diagnosis of the aforementioned tissues in their various states of health and disease.

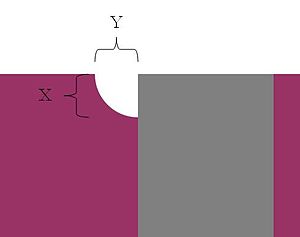
In implant dentistry, running room refers to the apico-coronal distance between the platform of a dental implant and the gingival margin. It is a critical factor in restorative implant dentistry because it is effectively the "vertical distance [available subgingivaly] to make a transition from the smaller diameter prosthetic platform of an implant to the larger cross-sectional cervical shape of the tooth being restored." The term was coined by Jonathan Zamzok, a Manhattan prosthodontist, in the late 1990s.
Peri-implant mucositis is defined as an inflammatory lesion of the peri-implant mucosa in the absence of continuing marginal bone loss.
Clinical attachment loss (CAL) is the predominant clinical manifestation and determinant of periodontal disease.

Bicon Dental Implants is a privately owned company located in Boston, MA. The company specializes in short dental implants that use a locking taper or cold welding connection to secure the abutment to the implant. Bicon is notable and worthy of mention for the following three reasons: First, Bicon implants are extremely short in length. The size of Bicon implants allow them to be placed in regions that are crowded with natural teeth and/or implants, or in regions that would otherwise require bone grafting. Second, the implants do not have the screw-form design typical of other available implants. Third, the abutments are connected to the implant via a locking taper. This is notable from both a medical and engineering standpoint as no other implant company offers an implant with a biological seal at the implant/abutment interface; almost all other implants possess an internal screw to connect their abutments.
A complete denture is a removable appliance used when all teeth within a jaw have been lost and need to be prosthetically replaced. In contrast to a partial denture, a complete denture is constructed when there are no more teeth left in an arch, hence it is an exclusively tissue-supported prosthesis. A complete denture can be opposed by natural dentition, a partial or complete denture, fixed appliances or, sometimes, soft tissues.

Overdenture is any removable dental prosthesis that covers and rests on one or more remaining natural teeth, the roots of natural teeth, and/or dental implants. It is one of the most practical measures used in preventive dentistry. Overdentures can be either tooth supported or implant supported. It is found to help in the preservation of alveolar bone and delay the process of complete edentulism.
![This dental radiograph displays two identical 5.0 mm diameter Biomet 3i tapered dental implants placed into the lower right mandible. The healing abutment on the more posterior implant [left] is platform matched (it shares the same 5.0 mm diameter as the implant platform), while the healing abutment on the more anterior implant [right] is platform switched (it possesses a 4.1 mm diameter). Platform switch.jpg](http://upload.wikimedia.org/wikipedia/commons/thumb/b/b6/Platform_switch.jpg/350px-Platform_switch.jpg)