The Diagnostic and Statistical Manual of Mental Disorders (DSM), published by the American Psychiatric Association (APA), offers a common language and standard criteria for the classification of mental disorders. It is used, or relied upon, by clinicians, researchers, psychiatric drug regulation agencies, health insurance companies, pharmaceutical companies, the legal system, and policy makers together with alternatives such as the ICD-10 Classification of Mental and Behavioural Disorders, produced by the WHO.

Dissociative identity disorder (DID), previously known as multiple personality disorder, is a mental disorder characterized by at least two distinct and relatively enduring personality states. This is accompanied by memory gaps, beyond what would be explained by ordinary forgetfulness. These states alternately show in a person's behavior; presentations, however, are variable. Other conditions which often occur in people with DID include borderline personality disorder (BPD), posttraumatic stress disorder (PTSD), depression, substance use disorders, self-harm, or anxiety.

Substance abuse, also known as drug abuse, is a patterned use of a drug in which the user consumes the substance in amounts or with methods which are harmful to themselves or others, and is a form of substance-related disorder. Widely differing definitions of drug abuse are used in public health, medical and criminal justice contexts. In some cases criminal or anti-social behaviour occurs when the person is under the influence of a drug, and long term personality changes in individuals may occur as well. In addition to possible physical, social, and psychological harm, use of some drugs may also lead to criminal penalties, although these vary widely depending on the local jurisdiction.

Alcohol abuse encompasses a spectrum of unhealthy alcohol drinking behaviors, ranging from binge drinking to alcohol dependence.
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. The diagnosis is made when the person has symptoms of both schizophrenia and a mood disorder—either bipolar disorder or depression—but does not meet the diagnostic criteria for schizophrenia or a mood disorder individually. The main criterion for the schizoaffective disorder diagnosis is the presence of psychotic symptoms for at least two weeks without any mood symptoms present. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, psychotic bipolar disorder, schizophreniform disorder or schizophrenia. It is imperative for providers to accurately diagnose patients, as treatment and prognosis differs greatly for each of these diagnoses.
Substance abuse, also known as drug abuse, is a patterned use of a substance (drug) in which the user consumes the substance in amounts or with methods which are harmful to themselves or others. The drugs used are often associated with levels of intoxication that alter judgment, perception, attention and physical control, not related with medical effects. It is often thought that the main abused substances are illegal drugs and alcohol; however it is becoming more common that prescription drugs and tobacco are a prevalent problem.
Alcohol dependence is a previous psychiatric diagnosis in which an individual is physically or psychologically dependent upon alcohol.

Problem gambling is an urge to gamble continuously despite harmful negative consequences or a desire to stop. Problem gambling is often defined by whether harm is experienced by the gambler or others, rather than by the gambler's behaviour. Severe problem gambling may be diagnosed as clinical pathological gambling if the gambler meets certain criteria. Pathological gambling is a common disorder that is associated with both social and family costs.
Sexual addiction, also known as sex addiction, is a state characterized by compulsive participation or engagement in sexual activity, particularly sexual intercourse, despite negative consequences.
Alcohol-related dementia (ARD) is a form of dementia caused by long-term, excessive consumption of alcoholic beverages, resulting in neurological damage and impaired cognitive function.
Dual diagnosis is the condition of suffering from a mental illness and a comorbid substance abuse problem. There is considerable debate surrounding the appropriateness of using a single category for a heterogeneous group of individuals with complex needs and a varied range of problems. The concept can be used broadly, for example depression and alcoholism, or it can be restricted to specify severe mental illness and substance misuse disorder, or a person who has a milder mental illness and a drug dependency, such as panic disorder or generalized anxiety disorder and is dependent on opioids. Diagnosing a primary psychiatric illness in substance abusers is challenging as drug abuse itself often induces psychiatric symptoms, thus making it necessary to differentiate between substance induced and pre-existing mental illness.

A person with polysubstance dependence is psychologically addicted to being in an intoxicated state without a preference for one particular substance. Although any combination of three drugs can be used, studies have shown that alcohol is commonly used with another substance. This is supported by one study on polysubstance use that separated participants who used multiple substances into groups based on their preferred drug. The three substances were cocaine, alcohol, and heroin, which implies that those three are very popular. Other studies have found that opiates, cannabis, amphetamines, hallucinogens, inhalants and benzodiazepines are often used in combination as well. The results of a long-term or longitudinal study on substance use led the researchers to observe that excessively using or relying on one drug increased the probability of excessively using or relying on another drug.
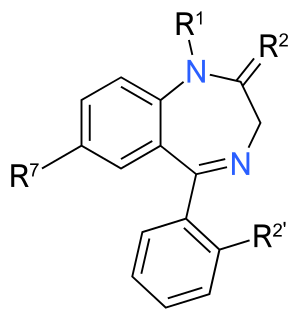
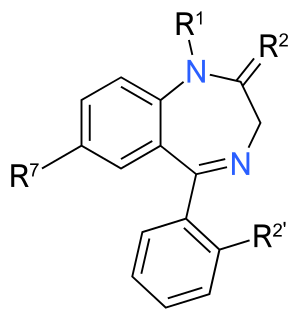
Benzodiazepine dependence is when one has developed one or more of either tolerance, withdrawal symptoms, drug seeking behaviors, such as continued use despite harmful effects, and maladaptive pattern of substance use, according to the DSM-IV. In the case of benzodiazepine dependence, however, the continued use seems to be associated with the avoidance of unpleasant withdrawal reaction rather than from the pleasurable effects of the drug. Benzodiazepine dependence develops with long-term use, even at low therapeutic doses, without the described dependence behavior.
Personality disorders (PD) are a class of mental disorders characterized by enduring maladaptive patterns of behavior, cognition, and inner experience, exhibited across many contexts and deviating from those accepted by the individual's culture. These patterns develop early, are inflexible, and are associated with significant distress or disability. The definitions may vary somewhat, according to source. Official criteria for diagnosing personality disorders are listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the fifth chapter of the International Classification of Diseases (ICD).

A substance use disorder (SUD), also known as a drug use disorder, is a medical condition in which the use of one or more substances leads to a clinically significant impairment or distress. Substance use disorders are characterized by an array of mental, physical, and behavioral symptoms that may cause problems related to loss of control, strain to one's interpersonal life, hazardous use, tolerance, and withdrawal. Drug classes that are involved in SUD include alcohol, phencyclidine, inhalants, stimulants, cannabis, "other hallucinogens", opioids, tobacco, and sedatives, hypnotics, and anxiolytics.
Cannabis use disorder (CUD), also known as cannabis addiction or marijuana addiction, is defined in the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and ICD-10 as the continued use of cannabis despite clinically significant impairment.
Gender-biased diagnosing is a controversial sociological observation which asserts that medical and psychological diagnosis may be influenced by the gender of the patient. Several studies have found evidence of differential diagnosis for patients with similar ailments but of different sexes.

Research data indicates that steroids affect the serotonin and dopamine neurotransmitter systems of the brain. In an animal study, male rats developed a conditioned place preference to testosterone injections into the nucleus accumbens, an effect blocked by dopamine antagonists, which suggests that androgen reinforcement is mediated by the brain. Moreover, testosterone appears to act through the mesolimbic dopamine system, a common substrate for drugs of abuse. Nonetheless, androgen reinforcement is not comparable to that of cocaine, nicotine, or heroin. Instead, testosterone resembles other mild reinforcers, such as caffeine, or benzodiazepines. The potential for androgen addiction remains to be determined.