In medicine, the ratio of physiologic dead space over tidal volume (VD/VT) is a routine measurement, expressing the ratio of dead-space ventilation (VD) to tidal ventilation (VT), as in physiologic research or the care of patients with respiratory disease. [1]
Dead space is the volume of air that is inhaled that does not take part in the gas exchange, because it either remains in the conducting airways or reaches alveoli that are not perfused or poorly perfused. In other words, not all the air in each breath is available for the exchange of oxygen and carbon dioxide. Mammals breathe in and out of their lungs, wasting that part of the inhalation which remains in the conducting airways where no gas exchange can occur.
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for artificial ventilation where mechanical means are used to assist or replace spontaneous breathing. This may involve a machine called a ventilator, or the breathing may be assisted manually by a suitably qualified professional, such as an anesthesiologist, registered nurse (RN), paramedic or other first responder, or in some parts of the United States, by a respiratory therapist (RT), by compressing a bag valve mask device.
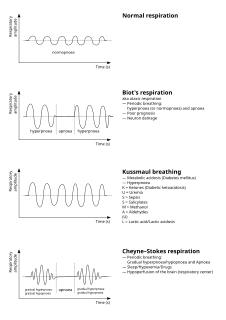
Cheyne–Stokes respiration is an abnormal pattern of breathing characterized by progressively deeper, and sometimes faster, breathing followed by a gradual decrease that results in a temporary stop in breathing called an apnea. The pattern repeats, with each cycle usually taking 30 seconds to 2 minutes. It is an oscillation of ventilation between apnea and hyperpnea with a crescendo-diminuendo pattern, and is associated with changing serum partial pressures of oxygen and carbon dioxide.
In pharmacology, the volume of distribution is the theoretical volume that would be necessary to contain the total amount of an administered drug at the same concentration that it is observed in the blood plasma. In other words, It is the ratio of amount of drug in a body (dose) to concentration of the drug that is measured in blood, plasma, and un-bound in interstitial fluid.
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
The void ratio of a mixture is the ratio of the volume of voids to volume of solids.
The respiratory exchange ratio (RER) is the ratio between the amount of carbon dioxide (CO2) produced in metabolism and oxygen (O2) used.
In respiratory physiology, the ventilation/perfusion ratio is a ratio used to assess the efficiency and adequacy of the matching of two variables:

Minute ventilation is the volume of gas inhaled or exhaled from a person's lungs per minute. It is an important parameter in respiratory medicine due to its relationship with blood carbon dioxide levels. It can be measured with devices such as a Wright respirometer or can be calculated from other known respiratory parameters. Although minute volume can be viewed as a unit of volume, it is usually treated in practice as a flow rate. Typical units involved are 0.5 L × 12 breaths/min = 6 L/min.
A pulmonary shunt refers to the passage of deoxygenated blood from the right side of the heart to the left without participation in gas exchange in the pulmonary capillaries. It is a pathological condition that results when the alveoli of the lungs are perfused with blood as normal, but ventilation fails to supply the perfused region. In other words, the ventilation/perfusion ratio is zero. A pulmonary shunt often occurs when the alveoli fill with fluid, causing parts of the lung to be unventilated although they are still perfused.
Lung compliance, or pulmonary compliance, is a measure of the lung's ability to stretch and expand. In clinical practice it is separated into two different measurements, static compliance and dynamic compliance. Static lung compliance is the change in volume for any given applied pressure. Dynamic lung compliance is the compliance of the lung at any given time during actual movement of air.
The alveolar gas equation is the method for calculating partial pressure of alveolar oxygen (PAO2). The equation is used in assessing if the lungs are properly transferring oxygen into the blood. The alveolar air equation is not widely used in clinical medicine, probably because of the complicated appearance of its classic forms. The partial pressure of oxygen (pO2) in the pulmonary alveoli is required to calculate both the alveolar-arterial gradient of oxygen and the amount of right-to-left cardiac shunt, which are both clinically useful quantities. However, it is not practical to take a sample of gas from the alveoli in order to directly measure the partial pressure of oxygen. The alveolar gas equation allows the calculation of the alveolar partial pressure of oxygen from data that is practically measurable. It was first characterized in 1946.
The multiple inert gas elimination technique (MIGET) is a medical technique used mainly in pulmonology that involves measuring the concentrations of various infused, inert gases in mixed venous blood, arterial blood, and expired gas of a subject. The technique quantifies true shunt, physiological dead space ventilation, ventilation versus blood flow (VA/Q) ratios, and diffusion limitation.
The Alveolar–arterial gradient, is a measure of the difference between the alveolar concentration (A) of oxygen and the arterial (a) concentration of oxygen. It is used in diagnosing the source of hypoxemia.
The Bohr equation, named after Danish physician Christian Bohr (1855–1911), describes the amount of physiological dead space in a person's lungs. This is given as a ratio of dead space to tidal volume. It differs from anatomical dead space as measured by Fowler's method as it includes alveolar dead space.
Respiratory inductance plethysmography (RIP) is a method of evaluating pulmonary ventilation by measuring the movement of the chest and abdominal wall.
The rapid shallow breathing index (RSBI) is a tool that is used in the weaning of mechanical ventilation on intensive care units. The RSBI is defined as the ratio of respiratory frequency to tidal volume (f/VT). People on a ventilator who cannot tolerate independent breathing tend to breathe rapidly and shallowly, and will therefore have a high RSBI.
ΔP is a mathematical term symbolizing a change (Δ) in pressure (P).
Fraction of inspired oxygen (FiO2) is the molar or volumetric fraction of oxygen in the inhaled gas. Medical patients experiencing difficulty breathing are provided with oxygen-enriched air, which means a higher-than-atmospheric FiO2. Natural air includes 21% oxygen, which is equivalent to FiO2 of 0.21. Oxygen-enriched air has a higher FiO2 than 0.21; up to 1.00 which means 100% oxygen. FiO2 is typically maintained below 0.5 even with mechanical ventilation, to avoid oxygen toxicity, but there are applications when up to 100% is routinely used.

The Interspiro DCSC is a semi-closed circuit nitrox rebreather manufactured by Interspiro of Sweden for military applications. Interspiro was formerly a division of AGA and has been manufacturing self-contained breathing apparatus for diving, firefighting and rescue applications since the 1950s.