Malaria is a mosquito-borne infectious disease that affects vertebrates. Human malaria causes symptoms that typically include fever, fatigue, vomiting, and headaches. In severe cases, it can cause jaundice, seizures, coma, or death. Symptoms usually begin 10 to 15 days after being bitten by an infected Anopheles mosquito. If not properly treated, people may have recurrences of the disease months later. In those who have recently survived an infection, reinfection usually causes milder symptoms. This partial resistance disappears over months to years if the person has no continuing exposure to malaria.
Antimalarial medications or simply antimalarials are a type of antiparasitic chemical agent, often naturally derived, that can be used to treat or to prevent malaria, in the latter case, most often aiming at two susceptible target groups, young children and pregnant women. As of 2018, modern treatments, including for severe malaria, continued to depend on therapies deriving historically from quinine and artesunate, both parenteral (injectable) drugs, expanding from there into the many classes of available modern drugs. Incidence and distribution of the disease is expected to remain high, globally, for many years to come; moreover, known antimalarial drugs have repeatedly been observed to elicit resistance in the malaria parasite—including for combination therapies featuring artemisinin, a drug of last resort, where resistance has now been observed in Southeast Asia. As such, the needs for new antimalarial agents and new strategies of treatment remain important priorities in tropical medicine. As well, despite very positive outcomes from many modern treatments, serious side effects can impact some individuals taking standard doses.

Plasmodium falciparum is a unicellular protozoan parasite of humans, and the deadliest species of Plasmodium that causes malaria in humans. The parasite is transmitted through the bite of a female Anopheles mosquito and causes the disease's most dangerous form, falciparum malaria. It is responsible for around 50% of all malaria cases. P. falciparum is therefore regarded as the deadliest parasite in humans. It is also associated with the development of blood cancer and is classified as a Group 2A (probable) carcinogen.
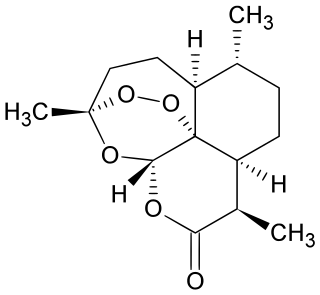
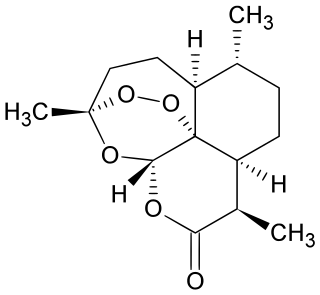
Artemisinin and its semisynthetic derivatives are a group of drugs used in the treatment of malaria due to Plasmodium falciparum. It was discovered in 1972 by Tu Youyou, who shared the 2015 Nobel Prize in Physiology or Medicine for her discovery. Artemisinin-based combination therapies (ACTs) are now standard treatment worldwide for P. falciparum malaria as well as malaria due to other species of Plasmodium. Artemisinin is extracted from the plant Artemisia annua an herb employed in Chinese traditional medicine. A precursor compound can be produced using a genetically engineered yeast, which is much more efficient than using the plant.

Artemether is a medication used for the treatment of malaria. The injectable form is specifically used for severe malaria rather than quinine. In adults, it may not be as effective as artesunate. It is given by injection in a muscle. It is also available by mouth in combination with lumefantrine, known as artemether/lumefantrine.

Artesunate (AS) is a medication used to treat malaria. The intravenous form is preferred to quinine for severe malaria. Often it is used as part of combination therapy, such as artesunate plus mefloquine. It is not used for the prevention of malaria. Artesunate can be given by injection into a vein, injection into a muscle, by mouth, and by rectum.
Artemether/lumefantrine, sold under the trade name Coartem among others, is a combination of the two medications artemether and lumefantrine. It is used to treat malaria caused by Plasmodium falciparum that is not treatable with chloroquine. It is not typically used to prevent malaria. It is taken by mouth.

The Drugs for Neglected Diseases initiative (DNDi) is a collaborative, patients' needs-driven, non-profit drug research and development (R&D) organization that is developing new treatments for neglected diseases, notably leishmaniasis, sleeping sickness, Chagas disease, malaria, filarial diseases, mycetoma, paediatric HIV, cryptococcal meningitis, hepatitis C, and dengue. DNDi's malaria activities were transferred to Medicines for Malaria Venture (MMV) in 2015.
Chlorproguanil/dapsone/artesunate was an experimental antimalarial treatment that entered Phase III clinical trials in 2006. Development was halted because it was associated with an increased risk of haemolytic anaemia in patients with glucose-6-phosphate dehydrogenase deficiency.

Dihydroartemisinin is a drug used to treat malaria. Dihydroartemisinin is the active metabolite of all artemisinin compounds and is also available as a drug in itself. It is a semi-synthetic derivative of artemisinin and is widely used as an intermediate in the preparation of other artemisinin-derived antimalarial drugs. It is sold commercially in combination with piperaquine and has been shown to be equivalent to artemether/lumefantrine.
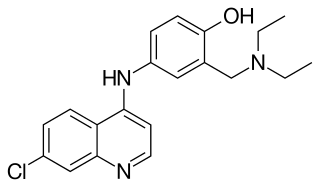
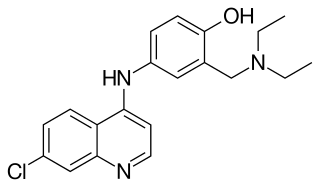
Amodiaquine (ADQ) is a medication used to treat malaria, including Plasmodium falciparum malaria when uncomplicated. It is recommended to be given with artesunate to reduce the risk of resistance. Due to the risk of rare but serious side effects, it is not generally recommended to prevent malaria. Though, the World Health Organization (WHO) in 2013 recommended use for seasonal preventive in children at high risk in combination with sulfadoxine and pyrimethamine.
Project 523 is a code name for a 1967 secret military project of the People's Republic of China to find antimalarial medications. Named after the date the project launched, 23 May, it addressed malaria, an important threat in the Vietnam War. At the behest of Ho Chi Minh, Prime Minister of North Vietnam, Zhou Enlai, the Premier of the People's Republic of China, convinced Mao Zedong, Chairman of the Chinese Communist Party, to start the mass project "to keep [the] allies' troops combat-ready", as the meeting minutes put it. More than 500 Chinese scientists were recruited. The project was divided into three streams. The one for investigating traditional Chinese medicine discovered and led to the development of a class of new antimalarial drugs called artemisinins. Launched during and lasting throughout the Cultural Revolution, Project 523 was officially terminated in 1981.
Atovaquone/proguanil, sold under the brand name Malarone among others, is a fixed-dose combination medication used to treat and prevent malaria, including chloroquine-resistant malaria. It contains atovaquone and proguanil. It is not recommended for severe or complicated malaria. It is taken by mouth.
Sulfadoxine/pyrimethamine, sold under the brand name Fansidar, is a combination medication used to treat malaria. It contains sulfadoxine and pyrimethamine. For the treatment of malaria it is typically used along with other antimalarial medication such as artesunate. In areas of Africa with moderate to high rates of malaria, three doses are recommended during the second and third trimester of pregnancy.
Piperaquine/dihydroartemisinin (DHA/PPQ), sold under the brand name Eurartesim among others, is a fixed dose combination medication used in the treatment of malaria. It is a combination of piperaquine and dihydroartemisinin. Specifically it is used for malaria of the P. falciparum and P. vivax types. It is taken by mouth.
Zhou Yiqing is a professor of medicine at the Institute of Microbiology and Epidemiology of the People's Liberation Army Academy of Military Medical Sciences. He was one of the scientists who participated in the Project 523 of the Chinese Government under Chairman Mao Zedong. The project resulted in the discovery of artemisinins, a class of antimalarial drugs, from the medicinal plant Artemisia annua.
Artesunate/mefloquine is a medication used to treat malaria. It is a fixed dose combination of artesunate and mefloquine. Specifically it is recommended to treat uncomplicated falciparum malaria. It is taken by mouth.
Artesunate/pyronaridine, sold under the brand name Pyramax, is a fixed-dose combination medication for the treatment of malaria. It can be used for malaria of both the P. falciparum and P. vivax types. It combines artesunate and pyronaridine. It is taken by mouth.