Sleep apnea is a sleep-related breathing disorder in which repetitive pauses in breathing, periods of shallow breathing, or collapse of the upper airway during sleep results in poor ventilation and sleep disruption. Each pause in breathing can last for a few seconds to a few minutes and occurs many times a night. A choking or snorting sound may occur as breathing resumes. Common symptoms include daytime sleepiness, snoring, and non restorative sleep despite adequate sleep time. Because the disorder disrupts normal sleep, those affected may experience sleepiness or feel tired during the day. It is often a chronic condition.
Tracheomalacia is a condition or incident where the cartilage that keeps the airway (trachea) open is soft such that the trachea partly collapses especially during increased airflow. This condition is most commonly seen in infants and young children. The usual symptom is stridor when a person breathes out. This is usually known as a collapsed windpipe.

Snoring is the vibration of respiratory structures and the resulting sound due to obstructed air movement during breathing while sleeping. The sound may be soft or loud and unpleasant. Snoring during sleep may be a sign, or first alarm, of obstructive sleep apnea (OSA). Research suggests that snoring is one of the factors of sleep deprivation.

Obesity hypoventilation syndrome (OHS) is a condition in which severely overweight people fail to breathe rapidly or deeply enough, resulting in low oxygen levels and high blood carbon dioxide (CO2) levels. The syndrome is often associated with obstructive sleep apnea (OSA), which causes periods of absent or reduced breathing in sleep, resulting in many partial awakenings during the night and sleepiness during the day. The disease puts strain on the heart, which may lead to heart failure and leg swelling.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.

Infant respiratory distress syndrome (IRDS), also called respiratory distress syndrome of newborn, or increasingly surfactant deficiency disorder (SDD), and previously called hyaline membrane disease (HMD), is a syndrome in premature infants caused by developmental insufficiency of pulmonary surfactant production and structural immaturity in the lungs. It can also be a consequence of neonatal infection and can result from a genetic problem with the production of surfactant-associated proteins.
Upper airway resistance syndrome (UARS) is a sleep disorder characterized by the narrowing of the airway that can cause disruptions to sleep. The symptoms include unrefreshing sleep, fatigue, sleepiness, chronic insomnia, and difficulty concentrating. UARS can be diagnosed by polysomnograms capable of detecting Respiratory Effort-related Arousals. It can be treated with lifestyle changes, functional orthodontics, surgery, mandibular repositioning devices or CPAP therapy. UARS is considered a variant of sleep apnea, although some scientists and doctors believe it to be a distinct disorder.
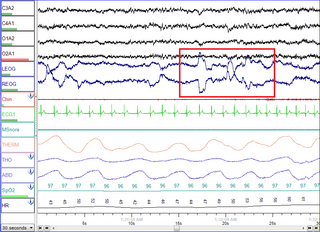
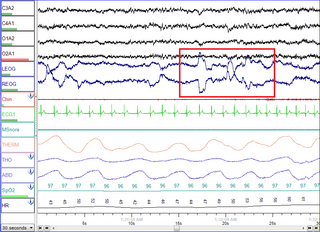
Polysomnography (PSG), a type of sleep study, is a multi-parameter study of sleep and a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated PSG. The name is derived from Greek and Latin roots: the Greek πολύς, the Latin somnus ("sleep"), and the Greek γράφειν.

A mandibi splint or mandibi advancement splint is a prescription custom-made medical device worn in the mouth used to treat sleep-related breathing disorders including: obstructive sleep apnea (OSA), snoring, and TMJ disorders. These devices are also known as mandibular advancement devices, sleep apnea oral appliances, oral airway dilators, and sleep apnea mouth guards.

Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation. While there are similarities with regard to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.

Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial obstruction of the upper airway leading to reduced or absent breathing during sleep. These episodes are termed "apneas" with complete or near-complete cessation of breathing, or "hypopneas" when the reduction in breathing is partial. In either case, a fall in blood oxygen saturation, a disruption in sleep, or both, may result. A high frequency of apneas or hypopneas during sleep may interfere with the quality of sleep, which – in combination with disturbances in blood oxygenation – is thought to contribute to negative consequences to health and quality of life. The terms obstructive sleep apnea syndrome (OSAS) or obstructive sleep apnea–hypopnea syndrome (OSAHS) may be used to refer to OSA when it is associated with symptoms during the daytime.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
Hypopnea is overly shallow breathing or an abnormally low respiratory rate. Hypopnea is defined by some to be less severe than apnea, while other researchers have discovered hypopnea to have a "similar if not indistinguishable impact" on the negative outcomes of sleep breathing disorders. In sleep clinics, obstructive sleep apnea syndrome or obstructive sleep apnea–hypopnea syndrome is normally diagnosed based on the frequent presence of apneas and/or hypopneas rather than differentiating between the two phenomena. Hypopnea is typically defined by a decreased amount of air movement into the lungs and can cause oxygen levels in the blood to drop. It commonly is due to partial obstruction of the upper airway.

Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year.

Catathrenia or nocturnal groaning is a sleep-related breathing disorder, consisting of end-inspiratory apnea and expiratory groaning during sleep. It describes a rare condition characterized by monotonous, irregular groans while sleeping. Catathrenia begins with a deep inspiration. The person with catathrenia holds her or his breath against a closed glottis, similar to the Valsalva maneuver. Expiration can be slow and accompanied by sound caused by vibration of the vocal cords or a simple rapid exhalation. Despite a slower breathing rate, no oxygen desaturation usually occurs. The moaning sound is usually not noticed by the person producing the sound, but it can be extremely disturbing to sleep partners. It appears more often during expiration REM sleep than in NREM sleep.
Hans Rudolph, was a pioneer in the development of respiratory equipment and supplies.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
Continuous spontaneous ventilation is any mode of mechanical ventilation where every breath is spontaneous.
Bubble CPAP is a non-invasive ventilation strategy for newborns with infant respiratory distress syndrome (IRDS). It is one of the methods by which continuous positive airway pressure (CPAP) is delivered to a spontaneously breathing newborn to maintain lung volumes during expiration. With this method, blended and humidified oxygen is delivered via short binasal prongs or a nasal mask and pressure in the circuit is maintained by immersing the distal end of the expiratory tubing in water. The depth to which the tubing is immersed underwater determines the pressure generated in the airways of the infant. As the gas flows through the system, it "bubbles" out and prevents buildup of excess pressures.