Safe sex is sexual activity using methods or contraceptive devices to reduce the risk of transmitting or acquiring sexually transmitted infections (STIs), especially HIV. "Safe sex" is also sometimes referred to as safer sex or protected sex to indicate that some safe sex practices do not eliminate STI risks. It is also sometimes used colloquially to describe methods aimed at preventing pregnancy that may or may not also lower STI risks.

Harm reduction, or harm minimization, refers to a range of public health policies designed to lessen the negative social and/or physical consequences associated with various human behaviors, both legal and illegal. Harm reduction is used to decrease negative consequences of recreational drug use and sexual activity without requiring abstinence, recognizing that those unable or unwilling to stop can still make positive change to protect themselves and others.

HIV/AIDS originated in Africa in the early 20th century and is a major public health concern and cause of death in many African countries. AIDS rates vary dramatically although the majority of cases are concentrated in Southern Africa. Although the continent is home to about 15.2 percent of the world's population, more than two-thirds of the total infected worldwide – some 35 million people – were Africans, of whom 15 million have already died. Sub-Saharan Africa alone accounted for an estimated 69 percent of all people living with HIV and 70 percent of all AIDS deaths in 2011. In the countries of sub-Saharan Africa most affected, AIDS has raised death rates and lowered life expectancy among adults between the ages of 20 and 49 by about twenty years. Furthermore, the life expectancy in many parts of Africa is declining, largely as a result of the HIV/AIDS epidemic with life-expectancy in some countries reaching as low as thirty-nine years.

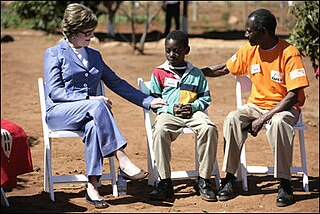
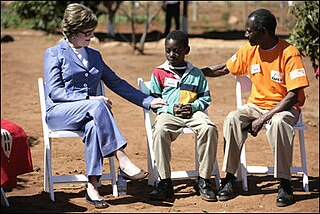
The United States President's Emergency Plan For AIDS Relief (PEPFAR) is a United States governmental initiative to address the global HIV/AIDS epidemic and help save the lives of those suffering from the disease. Launched by U.S. President George W. Bush in 2003, as of May 2020, PEPFAR has provided about $90 billion in cumulative funding for HIV/AIDS treatment, prevention, and research since its inception, making it the largest global health program focused on a single disease in history until the COVID-19 pandemic. PEPFAR is implemented by a combination of U.S. government agencies in over 50 countries and overseen by the Global AIDS Coordinator at the U.S. Department of State. As of 2021, PEPFAR has saved over 20 million lives, primarily in Sub-Saharan Africa.
Serosorting, also known as serodiscrimination, is the practice of using HIV status as a decision-making point in choosing sexual behavior. The term is used to describe the behavior of a person who chooses a sexual partner assumed to be of the same HIV serostatus in order to engage in unprotected sex with them for a reduced risk of acquiring or transmitting HIV/AIDS.

The first AIDS case identified in Brazil was in 1982. Infection rates climbed exponentially throughout the 1980s, and in 1990 the World Bank famously predicted 1,200,000 cases by 2000, approximately double the actual number that was later reported by the Brazilian Ministry of Health and most international organizations. South and Southeast have 75% or more of this infection. The Northeast has 33% of the population but only 10% of AIDS.
The Caribbean is the second-most affected region in the world in terms of HIV prevalence rates. Based on 2009 data, about 1.0 percent of the adult population is living with the disease, which is higher than any other region except Sub-Saharan Africa. Several factors influence this epidemic, including poverty, gender, sex tourism, and stigma. HIV incidence in the Caribbean declined 49% between 2001 and 2012. Different countries have employed a variety of responses to the disease, with a range of challenges and successes.
Abstinence-only sex education is a form of sex education that teaches not having sex outside of marriage. It often excludes other types of sexual and reproductive health education, such as birth control and safe sex. Comprehensive sex education, by contrast, covers the use of birth control and sexual abstinence.
Abstinence, be faithful, use a condom, also known as the ABC strategy or abstinence-plus sex education, also known as abstinence-based sex education, is a sex education policy based on a combination of "risk avoidance" and harm reduction which modifies the approach of abstinence-only sex education by including education about the value of partner reduction safe sex and birth control methods. Abstinence-only sex education is strictly to promote the sexual abstinence until marriage, and does not teach about safe sex or contraceptives. The abstinence-based sex education program is meant to stress abstinence and include information on safe sex practices. In general terms, this strategy of sex education is a compromise between abstinence-only education and comprehensive sex education. The ABC approach was developed in response to the growing epidemic of HIV/AIDS in Africa, and to prevent the spread of other sexually transmitted diseases. This approach has been credited by some with the falling numbers of those infected with AIDS in Uganda, Kenya and Zimbabwe, among others. From 1990 to 2001 the percentage of Ugandans living with AIDS fell from 15% to between 5 and 6%. This fall is believed to result from the employment of the ABC approach, especially reduction in the number of sex partners, called "Zero-Grazing" in Uganda.
The very high rate of HIV infection experienced in Uganda during the 1980s and early 1990s created an urgent need for people to know their HIV status. The only option available to them was offered by the National Blood Transfusion Service, which carries out routine HIV tests on all the blood that is donated for transfusion purposes. The great need for testing and counseling resulted in a group of local non-governmental organizations such as The AIDS Support Organisation (TASO), Uganda Red Cross, Nsambya Home Care, the National Blood Bank, the Uganda Virus Research Institute together with the Ministry of Health establishing the AIDS Information Centre in 1990. This organization worked to provide HIV testing and counseling services with the knowledge and consent of the client involved.
Angola has a large HIV/AIDS infected population, however, it has one of the lowest prevalence rates in the Southern Africa zone. The status of the HIV/AIDS epidemic in Angola is expected to change within the near future due to several forms of behavioral, cultural, and economic characteristics within the country such as lack of knowledge and education, low levels of condom use, the frequency of sex and number of sex partners, economic disparities and migration. There is a significant amount of work being done in Angola to combat the epidemic, but most aid is coming from outside of the country.
Kenya has a severe, generalized HIV epidemic, but in recent years, the country has experienced a notable decline in HIV prevalence, attributed in part to significant behavioral change and increased access to ARV. Adult HIV prevalence is estimated to have fallen from 10 percent in the late 1990s to about 4.8 percent in 2017. Women face considerably higher risk of HIV infection than men but have longer life expectancies than men when on ART. The 7th edition of AIDS in Kenya reports an HIV prevalence rate of eight percent in adult women and four percent in adult men. Populations in Kenya that are especially at risk include injecting drug users and people in prostitution, whose prevalence rates are estimated at 53 percent and 27 percent, respectively. Men who have sex with men (MSM) are also at risk at a prevalence of 18.2%. Other groups also include discordant couples however successful ARV-treatment will prevent transmission. Other groups at risk are prison communities, uniformed forces, and truck drivers.

Mozambique is a country particularly hard-hit by the HIV/AIDS epidemic. According to 2008 UNAIDS estimates, this southeast African nation has the 8th highest HIV rate in the world. With 1,600,000 Mozambicans living with HIV, 990,000 of which are women and children, Mozambique's government realizes that much work must be done to eradicate this infectious disease. To reduce HIV/AIDS within the country, Mozambique has partnered with numerous global organizations to provide its citizens with augmented access to antiretroviral therapy and prevention techniques, such as condom use. A surge toward the treatment and prevention of HIV/AIDS in women and children has additionally aided in Mozambique's aim to fulfill its Millennium Development Goals (MDGs). Nevertheless, HIV/AIDS has made a drastic impact on Mozambique; individual risk behaviors are still greatly influenced by social norms, and much still needs to be done to address the epidemic and provide care and treatment to those in need.
Since HIV/AIDS was first reported in Thailand in 1984, 1,115,415 adults had been infected as of 2008, with 585,830 having died since 1984. 532,522 Thais were living with HIV/AIDS in 2008. In 2009 the adult prevalence of HIV was 1.3%. As of 2016, Thailand had the highest prevalence of HIV in Southeast Asia at 1.1 percent, the 40th highest prevalence of 109 nations.
Vietnam faces a concentrated HIV epidemic.
Edward C. (Ted) Green is an American medical anthropologist working in public health and development. He was a senior research scientist at the Harvard School of Public Health and served as senior research scientist at the Harvard Center for Population and Development Studies for eight years, the last three years as director of the AIDS Prevention Project. He was later affiliated with the Department of Population and Reproductive Health at The Johns Hopkins University (2011–14) and the George Washington University as research professor. He was appointed to serve as a member of the Presidential Advisory Council on HIV/AIDS (2003–2007), and served on the Office of AIDS Research Advisory Council for the National Institutes of Health (2003–2006). Green serves on the board of AIDS.org and the Bonobo Conservation Initiative. and Medical Care Development.
The Catholic Church is a major provider of medical care to HIV/AIDS patients. Much of its work takes place in developing countries, although it has also had a presence in the global north. Its opposition to condoms, despite their effectiveness in preventing the spread of HIV, has invited criticism from public health officials and anti-AIDS activists.
The relationship between religion and HIV/AIDS has been an ongoing one, since the advent of the pandemic. Many faith communities have participated in raising awareness about HIV/AIDS, offering free treatment, as well as promoting HIV/AIDS testing and preventative measures. Christian denominations, such as Lutheranism and Methodism, have advocated for the observance of World AIDS Day to educate their congregations about the disease. Some Churches run voluntary blood testing camps and counselling centers to diagnose and help those affected by HIV/AIDS.
HIV prevention refers to practices that aim to prevent the spread of the human immunodeficiency virus (HIV). HIV prevention practices may be undertaken by individuals to protect their own health and the health of those in their community, or may be instituted by governments and community-based organizations as public health policies.
Uganda is one of the few Sub-Saharan African countries that has adopted abstinence-only sex education as an approach of sexual education that emphasizes abstinence from sexual intercourse until marriage as the only option. Abstinence-only sex education does not include joint curriculum covering other options including safe sex practices, family planning, and is espoused as the only sure way to avoid pregnancy and sexually transmitted infections. Uganda is commonly recognized as an exemplary case of lowering the rate of HIV prevalence Prevalence figures may have also been distorted by the lack of treatment, meaning that the percentage of infected is decreased by disproportionately early deaths. Abstinence-only sex education has been implemented and supported for this cause to a large degree in Uganda, to some controversy. Critics have questioned its effectiveness in lowering HIV/AIDS transmission. They have also highlighted discrimination, gender inequality and social stigma as the outcomes of the program in Uganda.