Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis. UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse. People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.

Fecal incontinence (FI), or in some forms, encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from a deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits. An estimated 2.2% of community-dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.
Incontinence or Incontinent may refer to:

Enuresis is a repeated inability to control urination. Use of the term is usually limited to describing people old enough to be expected to exercise such control. Involuntary urination is also known as urinary incontinence. The term "enuresis" comes from the Ancient Greek: ἐνούρησις, romanized: enoúrēsis.

Kegel exercise, also known as pelvic floor exercise, involves repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the "Kegel muscles". The exercise can be performed many times a day, for several minutes at a time but takes one to three months to begin to have an effect.

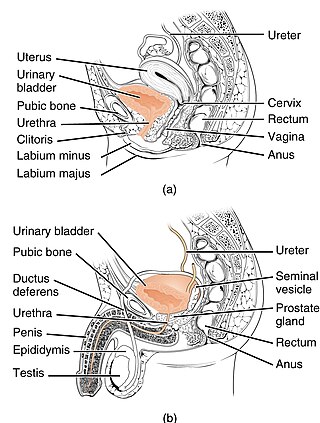
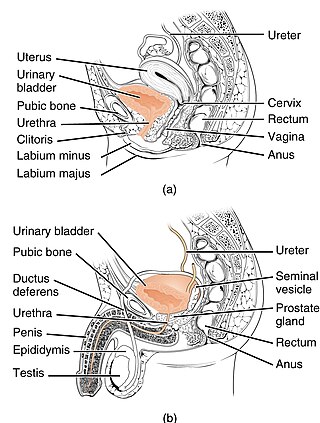
The pelvic floor or pelvic diaphragm is an anatomical location in the human body, which has an important role in urinary and anal continence, sexual function and support of the pelvic organs. The pelvic floor includes muscles, both skeletal and smooth, ligaments and fascia. and separates between the pelvic cavity from above, and the perineum from below. It is formed by the levator ani muscle and coccygeus muscle, and associated connective tissue.
An incontinence pad is a small, impermeable multi-layered sheet with high absorbency that is used in the incontinence and health-care industries as a precaution against fecal or urinary incontinence. It is generally made of cotton if washable, or nonwoven fabric paper if disposable. Incontinence diapers are a common incontinence pad. Incontinence pads are usually placed in an undergarment or on a bed or chair under a person. Incontinence pads are manufactured in light and heavy grades which offer a range of absorbencies, often referred to as a 'working capacity', which refers to the true absorbency an incontinence pad offers when in use. These sorts of pads can come as panty-liners, inserts, pads or even available as replacement underwear.
Percutaneous tibial nerve stimulation (PTNS), also referred to as posterior tibial nerve stimulation, is the least invasive form of neuromodulation used to treat overactive bladder (OAB) and the associated symptoms of urinary urgency, urinary frequency and urge incontinence. These urinary symptoms may also occur with interstitial cystitis and following a radical prostatectomy. Outside the United States, PTNS is also used to treat fecal incontinence.

An anal plug is a medical device that is often used to treat fecal incontinence, the accidental passing of bowel moments, by physically blocking involuntary loss of fecal material. Fecal material such as feces are solid remains of food that does not get digested in the small intestines; rather, it is broken down by bacteria in the large intestine. Anal plugs vary in design and composition, but they are typically single-use, intra-anal, disposable devices made out of soft materials to contain fecal material and prevent it from leaking out of the rectum. The idea of an anal insert for fecal incontinence was first evaluated in a study of 10 participants with three different designs of anal inserts.

A sacral nerve stimulator is a small device usually implanted in the buttocks of people who have problems with bladder and/or bowel control. This device is implanted in the buttock and connected to the sacral nerve S3 by a wire. The device uses sacral nerve stimulation to stop urges to defecate and urinate by sending signals to the sacral nerve. The patient is able to control their bladder and/or bowel via an external device similar to a remote control.
Sacral nerve stimulation, also termed sacral neuromodulation, is a type of medical electrical stimulation therapy.

A Malone antegrade continence enema (MACE), also known as an appendicostomy or Malone procedure, is a surgical procedure used to create a continent pathway proximal to the anus that facilitates fecal evacuation using enemas.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.

The International Continence Society (ICS) is a registered UK charity with a global health focus on the development in the field of incontinence.
National Association for Continence (NAFC) is a national, private, non-profit organization dedicated to improving the quality of life of people with incontinence, voiding dysfunction, and related pelvic floor disorders.

Overflow incontinence is a concept of urinary incontinence, characterized by the involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. This condition occurs in people who have a blockage of the bladder outlet, or when the muscle that expels urine from the bladder is too weak to empty the bladder normally. Overflow incontinence may also be a side effect of certain medications.
Coital incontinence (CI) is urinary leakage that occurs during either penetration or orgasm and can occur with a sexual partner or with masturbation. It has been reported to occur in 10% to 27% of sexually active women with urinary continence problems. There is evidence to suggest links between urinary leakage at penetration and urodynamic stress incontinence, and between urinary leakage at orgasm and detrusor overactivity.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.

An artificial urinary sphincter (AUS) is an implanted device to treat moderate to severe stress urinary incontinence, most commonly in men. The AUS is designed to supplement the function of the natural urinary sphincter that restricts urine flow out of the bladder.
Pelvic floor physical therapy (PFPT) is a specialty area within physical therapy focusing on the rehabilitation of muscles in the pelvic floor after injury or dysfunction. It can be used to address issues such as muscle weakness or tightness post childbirth, dyspareunia, vaginismus, vulvodynia, constipation, fecal or urinary incontinence, pelvic organ prolapse, and sexual dysfunction. Licensed physical therapists with specialized pelvic floor physical therapy training address dysfunction in individuals across the gender and sex spectra, though PFPT is often associated with women's health for its heavy focus on addressing issues of pelvic trauma after childbirth.