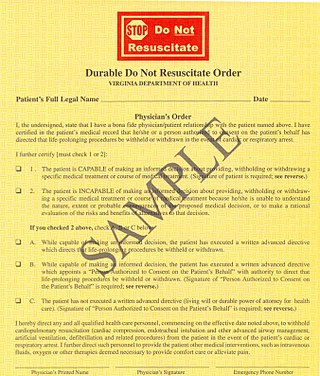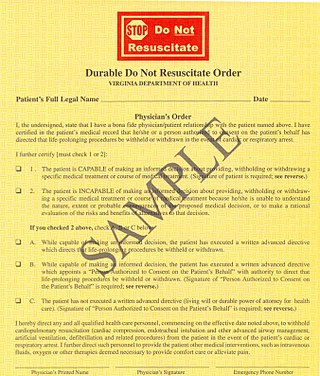
A do-not-resuscitate order (DNR), also known as Do Not Attempt Resuscitation (DNAR), Do Not Attempt Cardiopulmonary Resuscitation (DNACPR), no code or allow natural death, is a medical order, written or oral depending on the jurisdiction, indicating that a person should not receive cardiopulmonary resuscitation (CPR) if that person's heart stops beating. Sometimes these decisions and the relevant documents also encompass decisions around other critical or life-prolonging medical interventions. The legal status and processes surrounding DNR orders vary in different polities. Most commonly, the order is placed by a physician based on a combination of medical judgement and patient involvement.

Life support comprises the treatments and techniques performed in an emergency in order to support life after the failure of one or more vital organs. Healthcare providers and emergency medical technicians are generally certified to perform basic and advanced life support procedures; however, basic life support is sometimes provided at the scene of an emergency by family members or bystanders before emergency services arrive. In the case of cardiac injuries, cardiopulmonary resuscitation is initiated by bystanders or family members 25% of the time. Basic life support techniques, such as performing CPR on a victim of cardiac arrest, can double or even triple that patient's chance of survival. Other types of basic life support include relief from choking, staunching of bleeding by direct compression and elevation above the heart, first aid, and the use of an automated external defibrillator.
Palliative care is an interdisciplinary medical caregiving approach aimed at optimizing quality of life and mitigating suffering among people with serious, complex, and often terminal illnesses. Within the published literature, many definitions of palliative care exist. The World Health Organization (WHO) describes palliative care as "an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain, illnesses including other problems whether physical, psychosocial, and spiritual". In the past, palliative care was a disease specific approach, but today the WHO takes a broader patient-centered approach that suggests that the principles of palliative care should be applied as early as possible to any chronic and ultimately fatal illness. This shift was important because if a disease-oriented approach is followed, the needs and preferences of the patient are not fully met and aspects of care, such as pain, quality of life, and social support, as well as spiritual and emotional needs, fail to be addressed. Rather, a patient-centered model prioritizes relief of suffering and tailors care to increase the quality of life for terminally ill patients.

Intensive care medicine, also called critical care medicine, is a medical specialty that deals with seriously or critically ill patients who have, are at risk of, or are recovering from conditions that may be life-threatening. It includes providing life support, invasive monitoring techniques, resuscitation, and end-of-life care. Doctors in this specialty are often called intensive care physicians, critical care physicians, or intensivists.
The right to die is a concept based on the opinion that human beings are entitled to end their life or undergo voluntary euthanasia. Possession of the right to die is often bestowed with the understanding that a person with a terminal illness, incurable pain, or without the will to continue living should be allowed to end their own life, use assisted suicide, or decline life-prolonging treatment. The question of who, if anyone, may be empowered to make this decision is often the subject of debate.

Thanatology is the scientific study of death and the losses brought about as a result. It investigates the mechanisms and forensic aspects of death, such as bodily changes that accompany death and the postmortem period, as well as wider psychological and social aspects related to death. It is primarily an interdisciplinary study offered as a course of study at numerous colleges and universities.
In medicine, specifically in end-of-life care, palliative sedation is the palliative practice of relieving distress in a terminally ill person in the last hours or days of a dying person's life, usually by means of a continuous intravenous or subcutaneous infusion of a sedative drug, or by means of a specialized catheter designed to provide comfortable and discreet administration of ongoing medications via the rectal route.
Terminal illness or end-stage disease is a disease that cannot be cured or adequately treated and is expected to result in the death of the patient. This term is more commonly used for progressive diseases such as cancer, dementia or advanced heart disease than for injury. In popular use, it indicates a disease that will progress until death with near absolute certainty, regardless of treatment. A patient who has such an illness may be referred to as a terminal patient, terminally ill or simply as being terminal. There is no standardized life expectancy for a patient to be considered terminal, although it is generally months or less. Life expectancy for terminal patients is a rough estimate given by the physician based on previous data and does not always reflect true longevity. An illness which is lifelong but not fatal is a chronic condition.

Stephanie Keene, better known by the pseudonym Baby K, was an anencephalic baby who became the center of a major American court case and a debate among bioethicists.

An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine.
End-of-life care (EOLC) is health care provided in the time leading up to a person's death. End-of-life care can be provided in the hours, days, or months before a person dies and encompasses care and support for a person's mental and emotional needs, physical comfort, spiritual needs, and practical tasks.

Highland Hospital is a public hospital in Alameda County, Oakland, California. It is operated by the Alameda Health System. It is the primary trauma center and a county hospital in Alameda County.
The Liverpool Care Pathway for the Dying Patient (LCP) was a care pathway in the United Kingdom covering palliative care options for patients in the final days or hours of life. It was developed to help doctors and nurses provide quality end-of-life care, to transfer quality end-of-life care from the hospice to hospital setting. The LCP is no longer in routine use after public concerns regarding its nature. Alternative methodologies for Advance care planning are now in place to ensure patients are able to have dignity in their final hours of life. Hospitals were also provided cash incentives to achieve targets for the number of patients placed on the LCP.

In the United States, hospice care is a type and philosophy of end-of-life care which focuses on the palliation of a terminally ill patient's symptoms. These symptoms can be physical, emotional, spiritual, or social in nature. The concept of hospice as a place to treat the incurably ill has been evolving since the 11th century. Hospice care was introduced to the United States in the 1970s in response to the work of Cicely Saunders in the United Kingdom. This part of health care has expanded as people face a variety of issues with terminal illness. In the United States, it is distinguished by extensive use of volunteers and a greater emphasis on the patient's psychological needs in coming to terms with dying.

Hospice care is a type of health care that focuses on the palliation of a terminally ill patient's pain and symptoms and attending to their emotional and spiritual needs at the end of life. Hospice care prioritizes comfort and quality of life by reducing pain and suffering. Hospice care provides an alternative to therapies focused on life-prolonging measures that may be arduous, likely to cause more symptoms, or are not aligned with a person's goals.
Alameda Health System (AHS), formerly Alameda County Medical Center (ACMC), is an integrated public health care system organized as a public hospital authority.

End Game is a 2018 American short documentary film by Rob Epstein and Jeffrey Friedman about terminally ill patients in a San Francisco hospital meeting medical practitioners seeking to change the perception around life and death. The film was executive produced by Steven Ungerleider and Shoshana R. Ungerleider. It was released by Netflix.

The Good Nurse is a 2022 American thriller film starring Jessica Chastain and Eddie Redmayne, about the serial killer Charles Cullen and the fellow nurse who suspects him. The film is based on the 2013 true-crime book of the same name by Charles Graeber. It is directed by Tobias Lindholm and written by Krysty Wilson-Cairns. The film also stars Nnamdi Asomugha, Kim Dickens, and Noah Emmerich.

Shoshana Rebecca Ungerleider is an American medical doctor, journalist and film producer. She was educated at The University of Oregon and Oregon Health and Science University. As of June 2021, Ungerleider is the host of the TED Health Podcast, practices internal medicine, runs a non-profit that she founded, End Well, and during the COVID-19 pandemic, contributed regularly as a medical expert on CNN, MSNBC, CBS and Fox News.
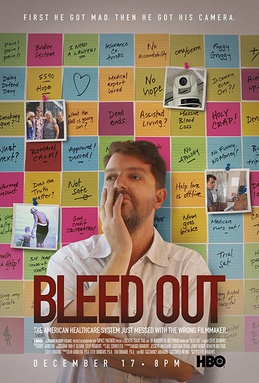
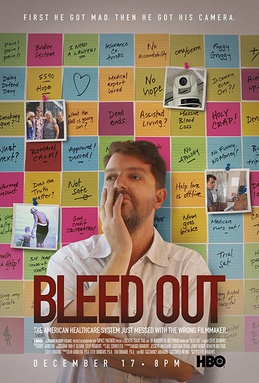
Bleed Out is a 2018 HBO feature documentary film that explores how an American family deals with the effects of medical malpractice. The film revolves around a ten-year journey, captured through archival footage, spy-cams, and interviews. Writer-director Steve Burrows reveals the ways his mother, Judie Burrows, was afflicted for the rest of her life due to a mistake during a partial hip surgery procedure.