An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.
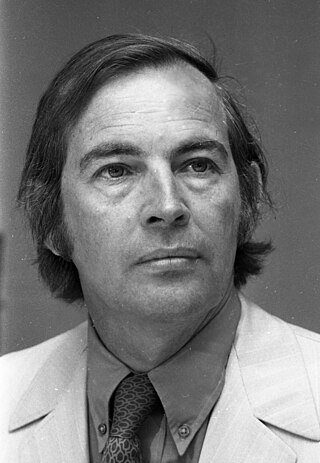
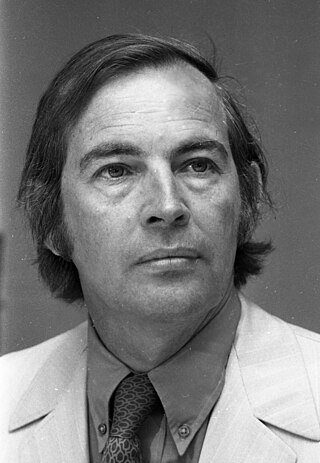
Christiaan Neethling Barnard was a South African cardiac surgeon who performed the world's first human-to-human heart transplant operation. On 3 December 1967, Barnard transplanted the heart of accident victim Denise Darvall into the chest of 54-year-old Louis Washkansky who regained full consciousness and was able to talk easily with his wife, before dying eighteen days later of pneumonia, largely brought on by the anti-rejection drugs that suppressed his immune system. Barnard had told Mr. and Mrs. Washkansky that the operation had an 80% chance of success, an assessment which has been criticised as misleading. Barnard's second transplant patient, Philip Blaiberg, whose operation was performed at the beginning of 1968, returned home from the hospital and lived for a year and a half.
Psychosomatic medicine is an interdisciplinary medical field exploring the relationships among social, psychological, behavioral factors on bodily processes and quality of life in humans and animals.
Clinical death is the medical term for cessation of blood circulation and breathing, the two criteria necessary to sustain the lives of human beings and of many other organisms. It occurs when the heart stops beating in a regular rhythm, a condition called cardiac arrest. The term is also sometimes used in resuscitation research.

Cardiopulmonary bypass (CPB) or heart-lung machine also called the pump or CPB pump is a machine that temporarily takes over the function of the heart and lungs during open-heart surgery by maintaining the circulation of blood and oxygen throughout the body. As such it is an extracorporeal device.

Extracorporeal membrane oxygenation (ECMO), is a form of extracorporeal life support, providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of oxygen, gas exchange or blood supply (perfusion) to sustain life. The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation. The device used is a membrane oxygenator, also known as an artificial lung.
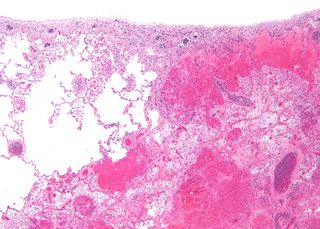
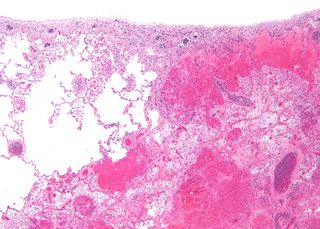
Infarction is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct (from the Latin infarctus, "stuffed into").

dextro-Transposition of the great arteries is a potentially life-threatening birth defect in the large arteries of the heart. The primary arteries are transposed.

Helen Brooke Taussig was an American cardiologist, working in Baltimore and Boston, who founded the field of pediatric cardiology. She is credited with developing the concept for a procedure that would extend the lives of children born with Tetralogy of Fallot. This concept was applied in practice as a procedure known as the Blalock-Thomas-Taussig shunt. The procedure was developed by Alfred Blalock and Vivien Thomas, who were Taussig's colleagues at the Johns Hopkins Hospital.

Pulmonary atresia is a congenital malformation of the pulmonary valve in which the valve orifice fails to develop. The valve is completely closed thereby obstructing the outflow of blood from the heart to the lungs. The pulmonary valve is located on the right side of the heart between the right ventricle and pulmonary artery. In a normal functioning heart, the opening to the pulmonary valve has three flaps that open and close.

Lung transplantation, or pulmonary transplantation, is a surgical procedure in which one or both lungs are replaced by lungs from a donor. Donor lungs can be retrieved from a living or deceased donor. A living donor can only donate one lung lobe. With some lung diseases, a recipient may only need to receive a single lung. With other lung diseases such as cystic fibrosis, it is imperative that a recipient receive two lungs. While lung transplants carry certain associated risks, they can also extend life expectancy and enhance the quality of life for those with end stage pulmonary disease.
Deep hypothermic circulatory arrest (DHCA) is a surgical technique in which the temperature of the body falls significantly and blood circulation is stopped for up to one hour. It is used when blood circulation to the brain must be stopped because of delicate surgery within the brain, or because of surgery on large blood vessels that lead to or from the brain. DHCA is used to provide a better visual field during surgery due to the cessation of blood flow. DHCA is a form of carefully managed clinical death in which heartbeat and all brain activity cease.
The Mustard procedure was developed in 1963 by Dr. William Mustard at the Hospital for Sick Children in Toronto, Ontario, Canada.
Targeted temperature management (TTM) previously known as therapeutic hypothermia or protective hypothermia is an active treatment that tries to achieve and maintain a specific body temperature in a person for a specific duration of time in an effort to improve health outcomes during recovery after a period of stopped blood flow to the brain. This is done in an attempt to reduce the risk of tissue injury following lack of blood flow. Periods of poor blood flow may be due to cardiac arrest or the blockage of an artery by a clot as in the case of a stroke.
Adrian Kantrowitz was an American cardiac surgeon whose team performed the world's second heart transplant attempt at Maimonides Medical Center in Brooklyn, New York on December 6, 1967. The infant lived for only six hours. At a press conference afterwards, Kantrowitz emphasized that he considered the operation to have been a failure.
James D. Hardy was a United States surgeon who performed the world's first lung transplant into John Russell, who lived 18 days. The transplant was performed at the University of Mississippi Medical Center in Jackson, Mississippi on June 11, 1963.

A heart transplant, or a cardiac transplant, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease when other medical or surgical treatments have failed. As of 2018, the most common procedure is to take a functioning heart, with or without both lungs, from a recently deceased organ donor and implant it into the patient. The patient's own heart is either removed and replaced with the donor heart or, much less commonly, the recipient's diseased heart is left in place to support the donor heart.
Boyd Rusia Rush was an American upholsterer who was the recipient of the world's first heart transplant on January 24, 1964, at University of Mississippi Medical Center in Jackson, Mississippi. Furthermore, Boyd's doctor James D. Hardy used a chimpanzee heart since no human donor heart was readily available. This heart beat in Rush's chest for approximately one hour, and then failed. Rush never regained consciousness.

Willis John Potts was an American pediatric surgeon and one of the earliest physicians to focus on the surgical treatment of heart problems in children. Potts set up one of the country's first pediatric surgery programs at Children's Memorial Hospital in Chicago.
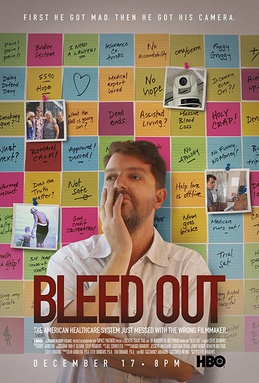
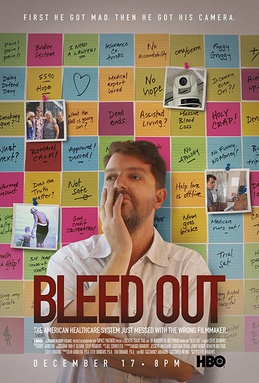
Bleed Out is a 2018 HBO feature documentary film that explores how an American family deals with the effects of medical malpractice. The film revolves around a ten-year journey, captured through archival footage, spy-cams, and interviews. Writer-director Steve Burrows reveals the ways his mother, Judie Burrows, was afflicted for the rest of her life due to a mistake during a partial hip surgery procedure.