Related Research Articles

Melanoma, also redundantly known as malignant melanoma, is a type of skin cancer that develops from the pigment-producing cells known as melanocytes. Melanomas typically occur in the skin, but may rarely occur in the mouth, intestines, or eye. In women, they most commonly occur on the legs, while in men, they most commonly occur on the back. About 25% of melanomas develop from moles. Changes in a mole that can indicate melanoma include an increase in size, irregular edges, change in color, itchiness, or skin breakdown.
A cancer vaccine is a vaccine that either treats existing cancer or prevents development of cancer. Vaccines that treat existing cancer are known as therapeutic cancer vaccines or tumor antigen vaccines. Some of the vaccines are "autologous", being prepared from samples taken from the patient, and are specific to that patient.

Cancer immunotherapy is the stimulation of the immune system to treat cancer, improving on the immune system's natural ability to fight the disease. It is an application of the fundamental research of cancer immunology and a growing subspecialty of oncology.

Ipilimumab, sold under the brand name Yervoy, is a monoclonal antibody medication that works to activate the immune system by targeting CTLA-4, a protein receptor that downregulates the immune system.
GP-100 can refer to
Oncophage, also known as cancer vaccine heat shock protein peptide complex-96 and cancer vaccine HSPPC-96, is a personalized cancer vaccine developed by the American biopharmaceutical company Antigenics Inc. that is evaluated in multiple clinical trials. It has been granted fast track and orphan drug designations from the US Food and Drug Administration for kidney cancer, metastatic melanoma, and glioma.
Cixutumumab (IMC-A12) is a human monoclonal antibody for the treatment of solid tumors.
James L. Gulley is an American cancer researcher and the Director of the Medical Oncology Service at National Cancer Institute.
Immunotransplant is a maneuver used to make vaccines more powerful. It refers to the process of infusing vaccine-primed T lymphocytes into lymphodepleted recipients for the purpose of enhancing the proliferation and function of those T cells and increasing immune protection induced by that vaccine.
Avax Technologies, Inc is a Philadelphia-based biotechnology company whose most advanced product candidate is MVax for melanoma. MVax is a cancer vaccine that received a Special Protocol Assessment agreement with the FDA in October 2006, and subsequently began a Phase III registration clinical trial in November 2007. In previous studies, MVax demonstrated a 5-year overall survival rate (OS)of 44% and response rate of 35%.
Glembatumumab vedotin is an antibody-drug conjugate (ADC) that targets cancer cells expressing transmembrane glycoprotein NMB (GPNMB).
SCIB1 is a genetically-engineered cancer vaccine being developed by Scancell Holdings Plc as a treatment for melanoma. Scancell's first cancer vaccine, SCIB1, is being developed for the treatment of melanoma and is in Phase I/II clinical trials. SCIB1 is a plasmid DNA which encodes a human antibody molecule engineered to express two cytotoxic T cell epitopes derived from the melanoma antigens Tyrosinase-Related Protein 2 (TRP2) and gp100 plus two helper T cell epitopes. Following immunisation, the engineered antibody is expressed and taken up by dendritic cells, resulting in the development of immune responses against tumour cells expressing the TRP2 and gp100 antigens. The major advantage of the Immunobody® technology is that the Fc component of the engineered antibody will be recognised by the high affinity CD64 receptor present on dendritic cells, leading to a significant enhancement of both the frequency and avidity of the T cell immune response. The induction of high avidity T cells against TRP-2 and gp100 destroys both primary and metastatic tumours, leading to longer progression free survival. Phase I/II clinical trial of SCIB1 Scancell is conducting a Phase I/II clinical trial of SCIB1, its DNA ImmunoBody® vaccine being developed for the treatment of melanoma. The trial is being carried out at clinical sites in Nottingham, Manchester, Guildford, Leeds and Southampton. . The trial is an open label, non-randomised study to determine the safety and tolerability of four doses of SCIB1 administered intramuscularly using an electroporation device. The study will also assess immune effects and anti-tumour activity in patients with melanoma. The trial is being conducted in patients with both unresected and resected disease. Patients with Stage III or Stage IV melanoma received up to five doses of the SCIB1 vaccine over a 6-month period. In addition some patients are being given long term treatment every 3–6 months for up to 5 years. The results to date have been highly encouraging. All 20 patients with resected tumours are still alive and only five have progressed. This compares very favourably with data from historical controls.
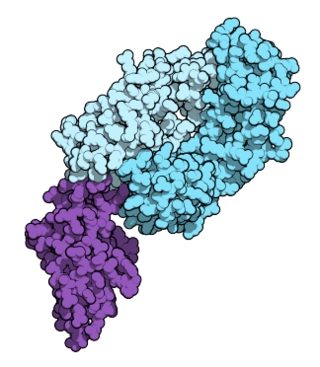
Glycoprotein 100, gp100 or Melanocyte protein PMEL is 661 amino acids long and is a type I transmembrane glycoprotein enriched in melanosomes, which are the melanin-producing organelles in melanocytes. This protein is involved in melanosome maturation.
Peptide-based synthetic vaccines, also called epitope vaccines, are subunit vaccines made from peptides. The peptides mimic the epitopes of the antigen that triggers direct or potent immune responses. Peptide vaccines can not only induce protection against infectious pathogens and non-infectious diseases but also be utilized as therapeutic cancer vaccines, where peptides from tumor-associated antigens are used to induce an effective anti-tumor T-cell response.

Vemurafenib (INN), sold under the brand name Zelboraf, is a medication used for the treatment of late-stage melanoma. It is an inhibitor of the B-Raf enzyme and was developed by Plexxikon.
Nivolumab, sold under the brand name Opdivo, is a medication used to treat a number of types of cancer. This includes melanoma, lung cancer, malignant pleural mesothelioma, renal cell carcinoma, Hodgkin lymphoma, head and neck cancer, urothelial carcinoma, colon cancer, esophageal squamous cell carcinoma, liver cancer, gastric cancer, and esophageal or gastroesophageal junction (GEJ) cancer. It is used by slow injection into a vein.

Pembrolizumab, sold under the brand name Keytruda, is a humanized antibody used in cancer immunotherapy that treats melanoma, lung cancer, head and neck cancer, Hodgkin lymphoma, stomach cancer, cervical cancer, and certain types of breast cancer. It is given by slow injection into a vein.
PROSTVAC is a cancer immunotherapy candidate in clinical development by Bavarian Nordic for the treatment of all prostate cancer although clinical trials are focusing on more advanced cases of metastatic castration-resistant prostate cancer (mCRPC). PROSTVAC is a vaccine designed to enable the immune system to recognize and attack prostate cancer cells by triggering a specific and targeted T cell immune response to cancer cells that express the tumor-associated antigen prostate-specific antigen (PSA).

Binimetinib, also known as Mektovi and ARRY-162, is an anti-cancer small molecule that was developed by Array Biopharma to treat various cancers. Binimetinib is a selective inhibitor of MEK, a central kinase in the tumor-promoting MAPK pathway. Inappropriate activation of the pathway has been shown to occur in many cancers. In June 2018 it was approved by the FDA in combination with encorafenib for the treatment of patients with unresectable or metastatic BRAF V600E or V600K mutation-positive melanoma.
The immune-related response criteria (irRC) is a set of published rules that define when tumors in cancer patients improve ("respond"), stay the same ("stabilize"), or worsen ("progress") during treatment, where the compound being evaluated is an immuno-oncology drug. Immuno-oncology, part of the broader field of cancer immunotherapy, involves agents which harness the body's own immune system to fight cancer. Traditionally, patient responses to new cancer treatments have been evaluated using two sets of criteria, the WHO criteria and the response evaluation criteria in solid tumors (RECIST). The immune-related response criteria, first published in 2009, arose out of observations that immuno-oncology drugs would fail in clinical trials that measured responses using the WHO or RECIST Criteria, because these criteria could not account for the time gap in many patients between initial treatment and the apparent action of the immune system to reduce the tumor burden.
References
- ↑ http://www.cancer.gov/drugdictionary/?CdrID=476335 [ bare URL ]
- ↑ http://www.cancer.gov/Templates/drugdictionary.aspx?CdrID=492712 [ bare URL ]
- ↑ "Re-induction with ipilimumab, gp100 peptide vaccine, or a combination of both from a phase III, randomized, double-blind, multicenter study of previously treated patients with unresectable stage III or IV melanoma". 2010.
- ↑ "Vaccine shows promise in advanced melanoma -study". Reuters. 30 May 2009.
- ↑ "BMS' Ipilimumab Proves Itself in Metastatic Melanoma Patients". 7 June 2010.