In the medical profession, a general practitioner (GP) is a medical doctor who treats acute and chronic illnesses and provides preventive care and health education to patients.
General practice is the name given in various nations, such as the United Kingdom, Australia and New Zealand, to the services provided by General practitioners. In some nations, such as the US, similar services may be described as family medicine or primary care. The term Primary Care in the UK may also include services provided by community pharmacy, optometrist, dental surgery and community hearing care providers. The balance of care between primary care and secondary care - which usually refers to hospital based services - varies from place to place, and with time. In many countries there are initiatives to move services out of hospitals into the community, in the expectation that this will save money and be more convenient.
Polyclinics in England were intended to offer a greater range of services than were offered by current general practitioner (GP) practices and local health centres. In addition to traditional GP services they would offer extended urgent care, healthy living services, community mental health services and social care, whilst being more accessible and less medicalised than hospitals. A variety of models were proposed, ranging from networks of existing clinics to larger premises with several colocated general practitioner (GP) practices, more extensive facilities and additional services provided by allied healthcare professionals.

The Royal Australian College of General Practitioners (RACGP) is the professional body for general practitioners (GPs) in Australia. The RACGP is responsible for maintaining standards for quality clinical practice, education and training, and research in Australian general practice. The RACGP represents over 40,000 members across metropolitan, urban, rural and remote Australia.
Yvonne Helen Carter was a British general practitioner and Dean of the Warwick Medical School, a post she took up in 2004, after being the Vice-Dean. Warwick Medical School is Britain's first medical school to only accept applications from graduates.
The Royal New Zealand College Of General Practitioners is a professional body and postgraduate educational institute that sets standards for general practice in New Zealand, providing research, assessment, ongoing education, advocacy and support for general practitioners and general practice.

Michael Dixon LVO, OBE, MA, FRCGP was chair of the NHS Alliance from 1998 to 2015 and is a past President of NHS Clinical Commissioners. He also chairs the College of Medicine. He is a Visiting Professor at University College London and the University of Westminster and National Clinical Champion for Social Prescribing.
Clare Mary Louise Francis Gerada, Lady Wessely is a London-based general practitioner who was chairperson of the Council of the Royal College of General Practitioners from 2010 to 2013. She has professional interests in mental health and substance misuse.

Clinical commissioning groups (CCGs) are NHS organisations set up by the Health and Social Care Act 2012 to organise the delivery of NHS services in England. The announcement that GPs would take over this commissioning role was made in the 2010 White Paper, "Equity and Excellence: Liberating the NHS". This was part of the Government's advertised desire to create a clinically-driven commissioning system that was more sensitive to the needs of patients. The 2010 White Paper became law under the Health and Social Care Act 2012 in March 2012. At the end of March 2013 there were 211 CCGs.
SSP Health is the largest provider of primary care GP services in the North West of England, one of only three such organisations in England serving more than 100,000 patients.
Out-of-hours services are the arrangements to provide access to healthcare at times when General Practitioner surgeries are closed; in the United Kingdom this is normally between 6.30pm and 8am, at weekends, at Bank Holidays and sometimes if the practice is closed for educational sessions.
The Modality Partnership is a large GP partnership formed in 2009. Such large practices are often described as a "super partnership". According to the King's Fund in 2016 it was one of England’s largest super-practices. In 2018 it had about 400,000 patients and was thought to be the largest practice in England.
Healthcare in the West Midlands is now the responsibility of five Clinical Commissioning Groups (CCG): Birmingham and Solihull; Sandwell and West Birmingham; Dudley; Wolverhampton; and Walsall.
The United Kingdom Clinical Pharmacy Association (UKCPA) is a not for profit organisation which promotes expert practice in medicines management for the benefit of patients, the public and professionals.
Private medicine in the UK, where there is universal state-funded healthcare, is a small niche market. Private provision of services for patients who pay should be distinguished from private providers who are paid by the NHS for services which are, as far as the patients are concerned, free.

Nick Harding OBE BSc FRCGP FRCP HonMFPH DRCOG DOccMed PGDIP(Cardiology) SFFLM, born 21 December 1969, is a British general practitioner, Chair of the NHS Sandwell and West Birmingham Clinical Commissioning Group, and Senior Clinical Advisor to NHS England.
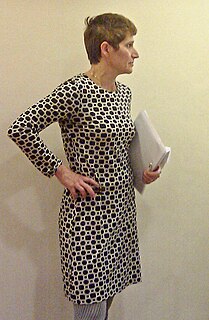
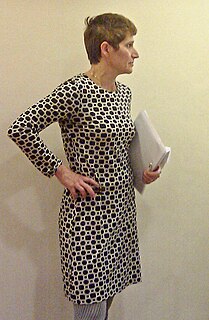
Helen Jayne Stokes-Lampard is a British medical academic and a general practitioner. She is Chair of the Royal College of General Practitioners (RCGP), the UK's largest Medical Royal College, representing over 52,000 family doctors across the UK. She has an interest in women's health.
GP Federations became popular among English General practitioners after 2010 as a means to exploit the opportunities - or mitigate the threats - posed by the Five Year Forward View proposals in the English NHS which envisaged delivering primary care at a larger scale than the traditional GP list. It is widely believed that ‘Practices cannot survive on their own – they have to look at ways of making themselves stronger.’ 15 sites were selected in December 2015 to test new enhanced primary care models serving populations of 30,000 to 50,000 patients. Some, but by no means all, Clinical Commissioning Groups have given financial support to encourage the formation of federations.
Nikita Kanani MBE is a general practitioner and the former chief clinical officer of the Bexley Clinical Commissioning Group. In 2018 she became the first woman to be director of primary care of the British National Health Service (NHS).
Primary care networks were introduced into the National Health Service in England as part of the NHS Long Term Plan, published in January 2019. The 2019 General Practitioner contract gave the opportunity for GP practices to join networks, each with between 30,000 and 50,000 patients. The stated aim is to create fully integrated community-based health services. By June 2019 1,259 primary care networks had been established across England, with an average population covered of about 42,000 patients, and including all but about 55 practices. About 25 had decided not to participate.