The humerus is a long bone in the arm that runs from the shoulder to the elbow. It connects the scapula and the two bones of the lower arm, the radius and ulna, and consists of three sections. The humeral upper extremity consists of a rounded head, a narrow neck, and two short processes. The body is cylindrical in its upper portion, and more prismatic below. The lower extremity consists of 2 epicondyles, 2 processes, and 3 fossae. As well as its true anatomical neck, the constriction below the greater and lesser tubercles of the humerus is referred to as its surgical neck due to its tendency to fracture, thus often becoming the focus of surgeons.
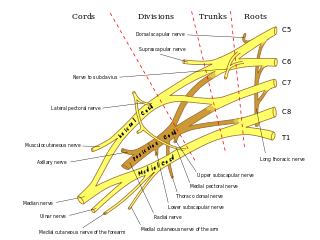
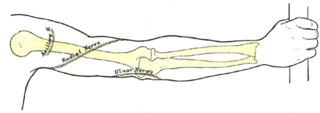
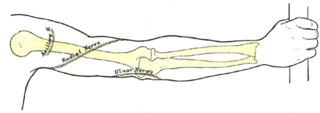
The ulnar nerve is a nerve that runs near the ulna, one of the two long bones in the forearm. The ulnar collateral ligament of elbow joint is in relation with the ulnar nerve. The nerve is the largest in the human body unprotected by muscle or bone, so injury is common. This nerve is directly connected to the little finger, and the adjacent half of the ring finger, innervating the palmar aspect of these fingers, including both front and back of the tips, perhaps as far back as the fingernail beds.

The deltoid muscle is the muscle forming the rounded contour of the human shoulder. It is also known as the 'common shoulder muscle', particularly in other animals such as the domestic cat. Anatomically, the deltoid muscle is made up of three distinct sets of muscle fibers, namely the
- anterior or clavicular part
- posterior or scapular part
- intermediate or acromial part
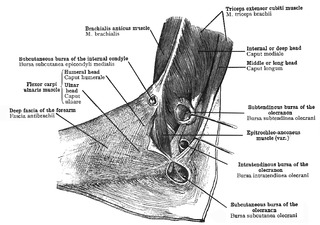
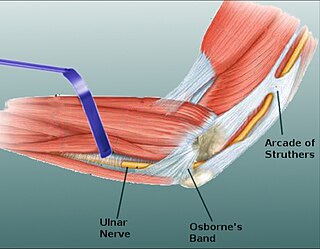
The cubital tunnel is a space of the dorsal medial elbow which allows passage of the ulnar nerve around the elbow. Persistent compression of the ulnar nerve in the cubital tunnel is known as cubital tunnel syndrome.
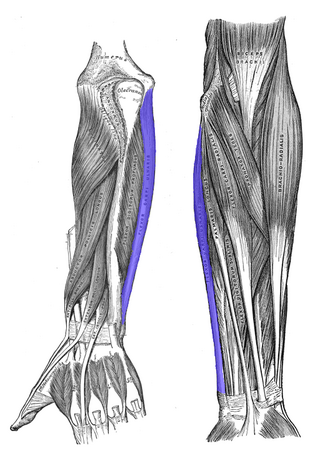
The flexor carpi ulnaris (FCU) is a muscle of the forearm that flexes and adducts at the wrist joint.

Tarsal tunnel syndrome (TTS) is a nerve compression syndrome or nerve entrapment syndrome causing a painful foot condition in which the tibial nerve is entrapped as it travels through the tarsal tunnel. The tarsal tunnel is found along the inner leg behind the medial malleolus. The posterior tibial artery, tibial nerve, and tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus muscles travel in a bundle through the tarsal tunnel. Inside the tunnel, the nerve splits into three segments. One nerve (calcaneal) continues to the heel, the other two continue on to the bottom of the foot. The tarsal tunnel is delineated by bone on the inside and the flexor retinaculum on the outside.

The teres major muscle is a muscle of the upper limb. It attaches to the scapula and the humerus and is one of the seven scapulohumeral muscles. It is a thick but somewhat flattened muscle.
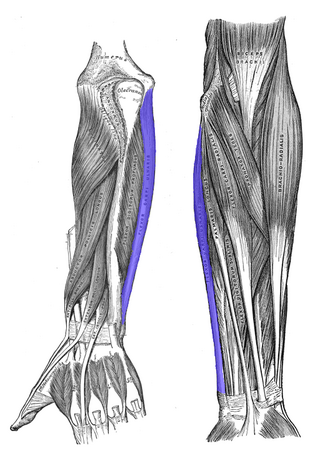
The pronator teres is a muscle that, along with the pronator quadratus, serves to pronate the forearm. It has two origins, at the medial humeral supracondylar ridge and the medial side of the coronoid process of the ulna and inserts near the middle of the radius.

The superior transverse ligament converts the suprascapular notch into a foramen or opening.

The suprascapular notch is a notch in the superior border of the scapula, just medial to the base of the coracoid process. It is converted into the suprascapular canal by the suprascapular ligament.

Cubitus varus is a varus deformity in which the extended forearm is deviated towards midline of the body.

Idiopathic ulnar neuropathy at the elbow is a condition where pressure on the ulnar nerve as it passes through the cubital tunnel causes ulnar neuropathy. The symptoms of neuropathy are paresthesia (tingling) and numbness primarily affecting the little finger and ring finger of the hand. Ulnar neuropathy can progress to weakness and atrophy of the muscles in the hand. Symptoms can be alleviated by the use of a splint to prevent the elbow from flexing while sleeping.

Ulnar neuropathy is a disorder involving the ulnar nerve. Ulnar neuropathy may be caused by entrapment of the ulnar nerve with resultant numbness and tingling. It may also cause weakness or paralysis of the muscles supplied by the nerve. Ulnar neuropathy may affect the elbow as cubital tunnel syndrome. At the wrist a similar neuropathy is ulnar tunnel syndrome.

A supracondylar humerus fracture is a fracture of the distal humerus just above the elbow joint. The fracture is usually transverse or oblique and above the medial and lateral condyles and epicondyles. This fracture pattern is relatively rare in adults, but is the most common type of elbow fracture in children. In children, many of these fractures are non-displaced and can be treated with casting. Some are angulated or displaced and are best treated with surgery. In children, most of these fractures can be treated effectively with expectation for full recovery. Some of these injuries can be complicated by poor healing or by associated blood vessel or nerve injuries with serious complications.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.

Injuries to the arm, forearm or wrist area can lead to various nerve disorders. One such disorder is median nerve palsy. The median nerve controls the majority of the muscles in the forearm. It controls abduction of the thumb, flexion of hand at wrist, flexion of digital phalanx of the fingers, is the sensory nerve for the first three fingers, etc. Because of this major role of the median nerve, it is also called the eye of the hand. If the median nerve is damaged, the ability to abduct and oppose the thumb may be lost due to paralysis of the thenar muscles. Various other symptoms can occur which may be repaired through surgery and tendon transfers. Tendon transfers have been very successful in restoring motor function and improving functional outcomes in patients with median nerve palsy.

The supracondylar process of the humerus is a variant bony projection on the anteromedial aspect of the upper arm bone (humerus), about 5–6 cm above the medial epicondyle. It is directed downward, forward and medially pointing to the medial epicondyle. A fibrous band, Struthers ligament, may connect this process to the medial epicondyle. This variation has a prevalence of 0.68% and is significantly more common in women than in men.
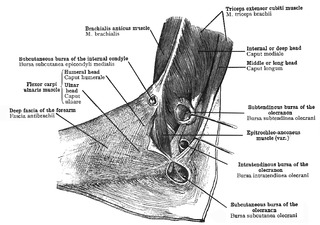
The epitrochleoanconeus muscle is a small accessory muscle of the arm which runs from the back of the inner condyle of the humerus over the ulnar nerve to the olecranon. The average prevalence of this muscle is 14.2% in healthy individuals.
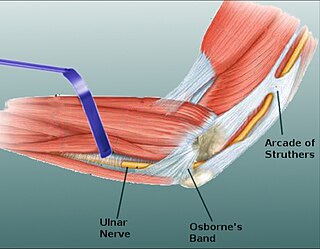
Osborne's ligament, also Osborne's band, Osborne's fascia, Osborne's arcade, arcuate ligament of Osborne, or the cubital tunnel retinaculum, refers to either the connective tissue which spans the humeral and ulnar heads of the flexor carpi ulnaris (FCU) or another distinct tissue located between the olecranon process of the ulna and the medial epicondyle of the humerus. It is named after Geoffrey Vaughan Osborne, a British orthopedic surgeon, who described the eponymous tissue in 1957.

Nerve entrapment involves a cascade of physiological changes caused by compression and tension. Some of these changes are irreversible. The magnitude and duration of the forces determines the extent of injury. In the acute form, mechanical injury and metabolic blocks impede nerve function. In the chronic form, there is a sequence of changes starting with a breakdown of the blood-nerve-barrier, followed by edema with connective tissue changes, followed by diffuse demyelination, and finally followed by axonmetesis. The injury will often be a mixed lesion where mild/moderate compression is a combination of a metabolic block and neuropraxia, while severe compression combines elements of neuropraxia and axonmetesis.