A headache is often present in patients with epilepsy. If the headache occurs in the vicinity of a seizure, it is defined as peri-ictal headache, which can occur either before (pre-ictal) or after (post-ictal) the seizure, to which the term ictal refers. An ictal headache itself may or may not be an epileptic manifestation. In the first case it is defined as ictal epileptic headache or simply epileptic headache. It is a real painful seizure, that can remain isolated or be followed by other manifestations of the seizure. On the other hand, the ictal non-epileptic headache is a headache that occurs during a seizure but it is not due to an epileptic mechanism. When the headache does not occur in the vicinity of a seizure it is defined as inter-ictal headache. In this case it is a disorder autonomous from epilepsy, that is a comorbidity.

An aura is a perceptual disturbance experienced by some with epilepsy or migraine. An epileptic aura is a seizure.
Long-term or "continuous" video-electroencephalography (EEG) monitoring is a diagnostic technique commonly used in patients with epilepsy. It involves the long-term hospitalization of the patient, typically for days or weeks, during which brain waves are recorded via EEG and physical actions are continuously monitored by video. In epileptic patients, this technique is typically used to capture brain activity during seizures. The information gathered can be used for initial prognosis or long-term care management.
Frontal lobe epilepsy (FLE) is a neurological disorder that is characterized by brief, recurring seizures that arise in the frontal lobes of the brain, often while the patient is sleeping. It is the second most common type of epilepsy after temporal lobe epilepsy (TLE), and is related to the temporal form by the fact that both forms are characterized by the occurrence of partial (focal) seizures. Partial seizures occurring in the frontal lobes can occur in one of two different forms: either simple partial seizures or complex partial seizures. The symptoms and clinical manifestations of frontal lobe epilepsy can differ depending on which specific area of the frontal lobe is affected.
Myoclonic epilepsy refers to a family of epilepsies that present with myoclonus. When myoclonic jerks are occasionally associated with abnormal brain wave activity, it can be categorized as myoclonic seizure. If the abnormal brain wave activity is persistent and results from ongoing seizures, then a diagnosis of myoclonic epilepsy may be considered.
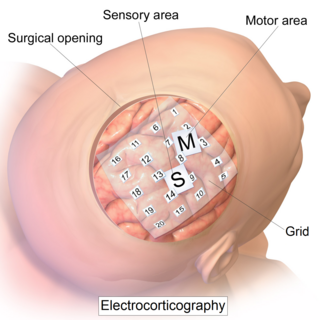
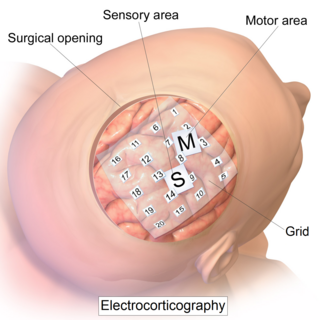
Electrocorticography (ECoG), or intracranial electroencephalography (iEEG), is a type of electrophysiological monitoring that uses electrodes placed directly on the exposed surface of the brain to record electrical activity from the cerebral cortex. In contrast, conventional electroencephalography (EEG) electrodes monitor this activity from outside the skull. ECoG may be performed either in the operating room during surgery or outside of surgery. Because a craniotomy is required to implant the electrode grid, ECoG is an invasive procedure.
The postictal state is the altered state of consciousness after an epileptic seizure. It usually lasts between 5 and 30 minutes, but sometimes longer in the case of larger or more severe seizures, and is characterized by drowsiness, confusion, nausea, hypertension, headache or migraine, and other disorienting symptoms. Additionally, emergence from this period is often accompanied by amnesia or other memory defects. It is during this period that the brain recovers from the trauma of the seizure.
Ring chromosome 20, ring-shaped chromosome 20 or r(20) syndrome is a rare human chromosome abnormality where the two arms of chromosome 20 fuse to form a ring chromosome. The syndrome is associated with epileptic seizures, behaviour disorders and intellectual disability.
Geschwind syndrome, also known as Gastaut-Geschwind, is a group of behavioral phenomena evident in some people with temporal lobe epilepsy. It is named for one of the first individuals to categorize the symptoms, Norman Geschwind, who published prolifically on the topic from 1973 to 1984. There is controversy surrounding whether it is a true neuropsychiatric disorder. Temporal lobe epilepsy causes chronic, mild, interictal changes in personality, which slowly intensify over time. Geschwind syndrome includes five primary changes; hypergraphia, hyperreligiosity, atypical sexuality, circumstantiality, and intensified mental life. Not all symptoms must be present for a diagnosis. Only some people with epilepsy or temporal lobe epilepsy show features of Geschwind syndrome.

A generalized tonic–clonic seizure, or GTCS, previously known as a Grand mal seizure, is a type of generalized seizure that produces bilateral, convulsive tonic and then clonic muscle contractions. Tonic-clonic seizures are the seizure type most commonly associated with epilepsy and seizures in general and the most common seizure associated with metabolic imbalances. It is a misconception that they are the sole type of seizure, as they are the main seizure type in approximately 10% of those with epilepsy.
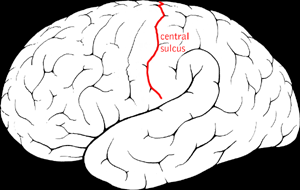
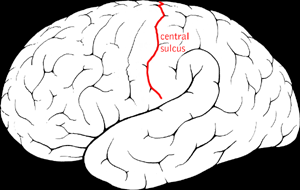
Benign Rolandic epilepsy or benign childhood epilepsy with centrotemporal spikes (BCECTS) is the most common epilepsy syndrome in childhood. Most children will outgrow the syndrome, hence the label benign. The seizures, sometimes referred to as sylvian seizures, start around the central sulcus of the brain.
Transient epileptic amnesia (TEA) is a rare but probably underdiagnosed neurological condition which manifests as relatively brief and generally recurring episodes of amnesia caused by underlying temporal lobe epilepsy. Though descriptions of the condition are based on fewer than 100 cases published in the medical literature, and the largest single study to date included 50 people with TEA, TEA offers considerable theoretical significance as competing theories of human memory attempt to reconcile its implications.
Panayiotopoulos syndrome is a common idiopathic childhood-related seizure disorder that occurs exclusively in otherwise normal children and manifests mainly with autonomic epileptic seizures and autonomic status epilepticus. An expert consensus has defined Panayiotopoulos syndrome as "a benign age-related focal seizure disorder occurring in early and mid-childhood. It is characterized by seizures, often prolonged, with predominantly autonomic symptoms, and by an EEG [electroencephalogram] that shows shifting and/or multiple foci, often with occipital predominance."
Ictal asystole is a rare occurrence for patients that have temporal lobe epilepsy. It can often be identified by loss of muscle tone or the presence of bilateral asymmetric jerky limb movements during a seizure, although ECG monitoring is necessary to provide a firm result. Ictal asystole and Ictal bradycardia can cause an epileptic patient to die suddenly.

Electroencephalography (EEG) is a method to record an electrogram of the electrical activity on the scalp that has been shown to represent the macroscopic activity of the surface layer of the brain underneath. It is typically non-invasive, with the electrodes placed along the scalp. Electrocorticography, involving invasive electrodes, is sometimes called "intracranial EEG".
Vertiginous epilepsy is infrequently the first symptom of a seizure, characterized by a feeling of vertigo. When it occurs, there is a sensation of rotation or movement that lasts for a few seconds before full seizure activity. While the specific causes of this disease are speculative there are several methods for diagnosis, the most important being the patient's recall of episodes. Most times, those diagnosed with vertiginous seizures are left to self-manage their symptoms or are able to use anti-epileptic medication to dampen the severity of their symptoms.
Epilepsy is a disorder in which nerve cell activity in the brain is disturbed, causing seizures.During a seizure, a person experiences abnormal behavior, symptoms, and sensations, sometimes including loss of consciousness. There are few symptoms between seizures. A seizure is a single occurrence, whereas epilepsy is a neurological condition characterized by two or more unprovoked seizures. Epilepsy is the most common childhood brain disorder in the United States. Nearly 3 million people have been diagnosed with this disease, while 450,000 of them are under the age of 17. Two thirds of the child population will overcome the side effects, including seizures, through treatment during adolescence. Some treatments include surgery, medication and therapy, surgery however is only done if the child has drug resistant epilepsy.
Idiopathic childhood occipital epilepsy of Gastaut (ICOE-G) is a pure but rare form of idiopathic occipital epilepsy that affects otherwise normal children and adolescents. It is classified amongst benign idiopathic childhood focal epilepsies such as rolandic epilepsy and Panayiotopoulos syndrome.
Ictal bradycardia is when people with temporal lobe epilepsy experience bradycardia with their seizures. Bradycardia is defined by a slower than normal heart rate, less than 60 bpm..

Occipital epilepsy is a neurological disorder that arises from excessive neural activity in the occipital lobe of the brain that may or may not be symptomatic. Occipital lobe epilepsy is fairly rare, and may sometimes be misdiagnosed as migraine when symptomatic. Epileptic seizures are the result of synchronized neural activity that is excessive, and may stem from a failure of inhibitory neurons to regulate properly.