Encephalomyelitis is inflammation of the brain and spinal cord. Various types of encephalomyelitis include:
Hemispherectomy is a neurosurgical procedure in which a cerebral hemisphere is removed or disconnected. It is used to treat a variety of refractory or drug-resistant seizure disorders (epilepsy).
Epilepsia partialis continua is a rare type of brain disorder in which a patient experiences recurrent motor epileptic seizures that are focal, and recur every few seconds or minutes for extended periods. It is sometimes called Kozhevnikov's epilepsia named after Russian psychiatrist Aleksei Yakovlevich Kozhevnikov who first described this type of epilepsy.

Glutamate receptors are synaptic and non synaptic receptors located primarily on the membranes of neuronal and glial cells. Glutamate is abundant in the human body, but particularly in the nervous system and especially prominent in the human brain where it is the body's most prominent neurotransmitter, the brain's main excitatory neurotransmitter, and also the precursor for GABA, the brain's main inhibitory neurotransmitter. Glutamate receptors are responsible for the glutamate-mediated postsynaptic excitation of neural cells, and are important for neural communication, memory formation, learning, and regulation.

In the field of neurology, temporal lobe epilepsy is an enduring brain disorder that causes unprovoked seizures from the temporal lobe. Temporal lobe epilepsy is the most common type of focal onset epilepsy among adults. Seizure symptoms and behavior distinguish seizures arising from the medial temporal lobe from seizures arising from the lateral (neocortical) temporal lobe. Memory and psychiatric comorbidities may occur. Diagnosis relies on electroencephalographic (EEG) and neuroimaging studies. Anticonvulsant medications, epilepsy surgery and dietary treatments may improve seizure control.
Juvenile myoclonic epilepsy (JME), also known as Janz syndrome or impulsive petit mal, is a form of hereditary, idiopathic generalized epilepsy, representing 5–10% of all epilepsy cases. Typically it first presents between the ages of 12 and 18 with myoclonic seizures. These events typically occur after awakening from sleep, during the evening or when sleep-deprived. JME is also characterized by generalized tonic–clonic seizures, and a minority of patients have absence seizures. It was first described by Théodore Herpin in 1857. Understanding of the genetics of JME has been rapidly evolving since the 1990s, and over 20 chromosomal loci and multiple genes have been identified. Given the genetic and clinical heterogeneity of JME some authors have suggested that it should be thought of as a spectrum disorder.
Epilepsy surgery involves a neurosurgical procedure where an area of the brain involved in seizures is either resected, ablated, disconnected or stimulated. The goal is to eliminate seizures or significantly reduce seizure burden. Approximately 60% of all people with epilepsy have focal epilepsy syndromes. In 15% to 20% of these patients, the condition is not adequately controlled with anticonvulsive drugs. Such patients are potential candidates for surgical epilepsy treatment.

Limbic encephalitis is a form of encephalitis, a disease characterized by inflammation of the brain. Limbic encephalitis is caused by autoimmunity: an abnormal state where the body produces antibodies against itself. Some cases are associated with cancer and some are not. Although the disease is known as "limbic" encephalitis, it is seldom limited to the limbic system and post-mortem studies usually show involvement of other parts of the brain. The disease was first described by Brierley and others in 1960 as a series of three cases. The link to cancer was first noted in 1968 and confirmed by later investigators.
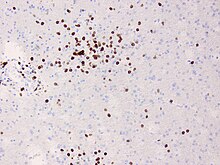
Anti-glutamate receptor antibodies are autoantibodies detected in serum and/or cerebrospinal fluid samples of a variety of disorders such as encephalitis, epilepsy and ataxia. Clinical and experimental studies starting around the year 2000 suggest that these antibodies are not simply epiphenomena and are involved in autoimmune disease pathogenesis.

Glutamate ionotropic receptor kainate type subunit 2, also known as ionotropic glutamate receptor 6 or GluR6, is a protein that in humans is encoded by the GRIK2 gene.

Leucine-rich, glioma inactivated 1, also known as LGI1, is a protein which in humans is encoded by the LGI1 gene. It may be a metastasis suppressor.

Anti-NMDA receptor encephalitis is a type of brain inflammation caused by antibodies. Early symptoms may include fever, headache, and feeling tired. This is then typically followed by psychosis which presents with false beliefs (delusions) and seeing or hearing things that others do not see or hear (hallucinations). People are also often agitated or confused. Over time, seizures, decreased breathing, and blood pressure and heart rate variability typically occur. In some cases, patients may develop catatonia.
Febrile infection-related epilepsy syndrome (FIRES), is onset of severe seizures following a febrile illness in someone who was previously healthy. The seizures may initially be focal; however, often become tonic-clonic. Complications often include intellectual disability, behavioral problems, and ongoing seizures.
James O. McNamara is an American neurologist and neuroscientist, known for his research of epileptogenesis, the process underlying development and progression of epilepsy. He is the Duke School of Medicine Professor of Neuroscience in the Departments of Neurobiology, Neurology, and Pharmacology and Cancer Biology at Duke University. He served as chair of the Department of Neurobiology at Duke from 2002 to 2011
People with epilepsy may be classified into different syndromes based on specific clinical features. These features include the age at which seizures begin, the seizure types, and EEG findings, among others. Identifying an epilepsy syndrome is useful as it helps determine the underlying causes as well as deciding what anti-seizure medication should be tried. Epilepsy syndromes are more commonly diagnosed in infants and children. Some examples of epilepsy syndromes include benign rolandic epilepsy, childhood absence epilepsy and juvenile myoclonic epilepsy. Severe syndromes with diffuse brain dysfunction caused, at least partly, by some aspect of epilepsy, are also referred to as epileptic encephalopathies. These are associated with frequent seizures that are resistant to treatment and severe cognitive dysfunction, for instance Lennox-Gastaut syndrome and West syndrome.

Autoimmune encephalitis (AIE) is a type of encephalitis, and one of the most common causes of noninfectious encephalitis. It can be triggered by tumors, infections, or it may be cryptogenic. The neurological manifestations can be either acute or subacute and usually develop within six weeks. The clinical manifestations include behavioral and psychiatric symptoms, autonomic disturbances, movement disorders, and seizures.
Anti-VGKC-complex encephalitis are caused by antibodies against the voltage gated potassium channel-complex (VGKC-complex) and are implicated in several autoimmune conditions including limbic encephalitis, epilepsy and neuromyotonia.

Svetlana Dambinova is a Russian neuroscientist, Doctor of Biological Sciences, Distinguished Professor at Laboratory of biomarkers at Medical Center "DeKalb", Atlanta, USA. Dambinova was awarded as Honored Worker of Science of the Republic of Buryatia (1996) and Russian Federation (1998). Known in the world for research of glutamate receptors. The Head of the project of the International Department of Neurology SPBGMU them. Acad. Pavlov's.
Drug-resistant epilepsy (DRE), also known as refractory epilepsy, intractable epilepsy, or pharmacoresistant epilepsy, is diagnosed following a failure of adequate trials of two tolerated and appropriately chosen and used antiepileptic drugs (AEDs) to achieve sustained seizure freedom. The probability that the next medication will achieve seizure freedom drops with every failed AED. For example, after two failed AEDs, the probability that the third will achieve seizure freedom is around 4%. Drug-resistant epilepsy is commonly diagnosed after several years of uncontrolled seizures, however, in most cases, it is evident much earlier. Approximately 30% of people with epilepsy have a drug-resistant form.
Anti-IgLON5 disease is a neurodegenerative autoimmune disease. It is marked by parasomnias and chorea - an involuntary movement disorder.