Related Research Articles

Stevens–Johnson syndrome (SJS) is a type of severe skin reaction. Together with toxic epidermal necrolysis (TEN) and Stevens–Johnson/toxic epidermal necrolysis (SJS/TEN), it forms a spectrum of disease, with SJS being less severe. Erythema multiforme (EM) is generally considered a separate condition. Early symptoms of SJS include fever and flu-like symptoms. A few days later, the skin begins to blister and peel, forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia and multiple organ failure.

Panniculitis is a group of diseases whose hallmark is inflammation of subcutaneous adipose tissue. Symptoms include tender skin nodules, and systemic signs such as weight loss and fatigue.

Lichen planus (LP) is a chronic inflammatory and autoimmune disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, but is named for its appearance. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. The hue may be gray-brown in people with darker skin. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Livedo reticularis is a common skin finding consisting of a mottled reticulated vascular pattern that appears as a lace-like purplish discoloration of the skin. The discoloration is caused by reduction in blood flow through the arterioles that supply the cutaneous capillaries, resulting in deoxygenated blood showing as blue discoloration. This can be a secondary effect of a condition that increases a person's risk of forming blood clots, including a wide array of pathological and nonpathological conditions. Examples include hyperlipidemia, microvascular hematological or anemia states, nutritional deficiencies, hyper- and autoimmune diseases, and drugs/toxins.

Sweet syndrome (SS), or acute febrile neutrophilic dermatosis, is a skin disease characterized by the sudden onset of fever, an elevated white blood cell count, and tender, red, well-demarcated papules and plaques that show dense infiltrates by neutrophil granulocytes on histologic examination.
Discoid lupus erythematosus (DLE) is an uncommon autoimmune disease of the basal cell layer of the skin. It occurs in humans and cats, more frequently occurring in dogs. It was first described in dogs by Griffin and colleagues in 1979. DLE is one form of cutaneous lupus erythematosus (CLE). DLE occurs in dogs in two forms: a classical facial predominant form or generalized with other areas of the body affected. Other non-discoid variants of CLE include vesicular CLE, exfoliative CLE and mucocutaneous CLE. It does not progress to systemic lupus erythematosus (SLE) in dogs. SLE can also have skin symptoms, but it appears that the two are either separate diseases. DLE in dogs differs from SLE in humans in that plasma cells predominate histologically instead of T lymphocytes. Because worsening of symptoms occurs with increased ultraviolet light exposure, sun exposure most likely plays a role in DLE, although certain breeds (see below) are predisposed. After pemphigus foliaceus, DLE is the second most common autoimmune skin disease in dogs.

Necrolytic migratory erythema is a red, blistering rash that spreads across the skin. It particularly affects the skin around the mouth and distal extremities; but may also be found on the lower abdomen, buttocks, perineum, and groin. It is strongly associated with glucagonoma, a glucagon-producing tumor of the pancreas, but is also seen in a number of other conditions including liver disease and intestinal malabsorption.
Desquamative gingivitis is an erythematous (red), desquamatous (shedding) and ulcerated appearance of the gums. It is a descriptive term and can be caused by several different disorders.

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a scaly and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.

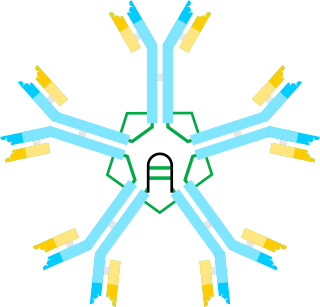
Lupus erythematosus is a collection of autoimmune diseases in which the human immune system becomes hyperactive and attacks healthy tissues. Symptoms of these diseases can affect many different body systems, including joints, skin, kidneys, blood cells, heart, and lungs. The most common and most severe form is systemic lupus erythematosus.
Isolated primary immunoglobulin M deficiency is a poorly defined dysgammaglobulinemia characterized by decreased levels of IgM while levels of other immunoglobulins are normal. The immunodeficiency has been associated with some clinical disorders including recurrent infections, atopy, Bloom's syndrome, celiac disease, systemic lupus erythematosus and malignancy, but, surprisingly, SIgMD seems to also occur in asymptomatic individuals. High incidences of recurrent upper respiratory tract infections (77%), asthma (47%) and allergic rhinitis (36%) have also been reported. SIgMD seems to be a particularly rare antibody deficiency with a reported prevalence between 0.03% and 0.1%.

In medicine, a drug eruption is an adverse drug reaction of the skin. Most drug-induced cutaneous reactions are mild and disappear when the offending drug is withdrawn. These are called "simple" drug eruptions. However, more serious drug eruptions may be associated with organ injury such as liver or kidney damage and are categorized as "complex". Drugs can also cause hair and nail changes, affect the mucous membranes, or cause itching without outward skin changes.
Pemphigus erythematosus is simply a localized form of pemphigus foliaceus with features of lupus erythematosus.
Chilblain lupus erythematosus was initially described by Hutchinson in 1888 as an uncommon manifestation of chronic cutaneous lupus erythematosus. Chilblain lupus erythematosus is characterized by a rash that primarily affects acral surfaces that are frequently exposed to cold temperatures, such as the toes, fingers, ears, and nose. The rash is defined by oedematous skin, nodules, and tender plaques with a purple discoloration.
Lupus erythematosus panniculitis presents with subcutaneous nodules that are commonly firm, sharply defined and nontender.
Palisaded neutrophilic and granulomatous dermaititis (PNGS) is usually associated with a well-defined connective tissue disease, lupus erythematosus or rheumatoid arthritis most commonly, and often presents with eroded or ulcerated symmetrically distributed umbilicated papules or nodules on the elbows.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.

Lupus vasculitis is one of the secondary vasculitides that occurs in approximately 50% of patients with systemic lupus erythematosus (SLE).
Cutaneous manifestations of COVID-19 are characteristic signs or symptoms of the Coronavirus disease 2019 that occur in the skin. The American Academy of Dermatology reports that skin lesions such as morbilliform, pernio, urticaria, macular erythema, vesicular purpura, papulosquamous purpura and retiform purpura are seen in people with COVID-19. Pernio-like lesions were more common in mild disease while retiform purpura was seen only in critically ill patients. The major dermatologic patterns identified in individuals with COVID-19 are urticarial rash, confluent erythematous/morbilliform rash, papulovesicular exanthem, chilbain-like acral pattern, livedo reticularis and purpuric "vasculitic" pattern. Chilblains and Multisystem inflammatory syndrome in children are also cutaneous manifestations of COVID-19.
References
- ↑ Child FJ, Kapur N, Creamer D, Kobza Black A (March 1999). "Rowell's syndrome". Clinical and Experimental Dermatology. 24 (2): 74–7. doi:10.1046/j.1365-2230.1999.00422.x. PMID 10233657. S2CID 41222604.
- ↑ Rowell's syndrome. http://www.casereports.in/articles/5/1/Rowells-syndrome.html