Related Research Articles

Positron emission tomography (PET) is a functional imaging technique that uses radioactive substances known as radiotracers to visualize and measure changes in metabolic processes, and in other physiological activities including blood flow, regional chemical composition, and absorption. Different tracers are used for various imaging purposes, depending on the target process within the body.
Aripiprazole, sold under the brand names Abilify and Aristada, among others, is an atypical antipsychotic. It is primarily used in the treatment of schizophrenia and bipolar disorder; other uses include as an add-on treatment in major depressive disorder and obsessive compulsive disorder (OCD), tic disorders, and irritability associated with autism. Aripiprazole is taken by mouth or via injection into a muscle. A Cochrane review found low-quality evidence of effectiveness in treating schizophrenia.
The dopamine hypothesis of schizophrenia or the dopamine hypothesis of psychosis is a model that attributes the positive symptoms of schizophrenia to a disturbed and hyperactive dopaminergic signal transduction. The model draws evidence from the observation that a large number of antipsychotics have dopamine-receptor antagonistic effects. The theory, however, does not posit dopamine overabundance as a complete explanation for schizophrenia. Rather, the overactivation of D2 receptors, specifically, is one effect of the global chemical synaptic dysregulation observed in this disorder.

Dopamine receptors are a class of G protein-coupled receptors that are prominent in the vertebrate central nervous system (CNS). Dopamine receptors activate different effectors through not only G-protein coupling, but also signaling through different protein interactions. The neurotransmitter dopamine is the primary endogenous ligand for dopamine receptors.

A dopamine antagonist, also known as an anti-dopaminergic and a dopamine receptor antagonist (DRA), is a type of drug which blocks dopamine receptors by receptor antagonism. Most antipsychotics are dopamine antagonists, and as such they have found use in treating schizophrenia, bipolar disorder, and stimulant psychosis. Several other dopamine antagonists are antiemetics used in the treatment of nausea and vomiting.
Neuropharmacology is the study of how drugs affect function in the nervous system, and the neural mechanisms through which they influence behavior. There are two main branches of neuropharmacology: behavioral and molecular. Behavioral neuropharmacology focuses on the study of how drugs affect human behavior (neuropsychopharmacology), including the study of how drug dependence and addiction affect the human brain. Molecular neuropharmacology involves the study of neurons and their neurochemical interactions, with the overall goal of developing drugs that have beneficial effects on neurological function. Both of these fields are closely connected, since both are concerned with the interactions of neurotransmitters, neuropeptides, neurohormones, neuromodulators, enzymes, second messengers, co-transporters, ion channels, and receptor proteins in the central and peripheral nervous systems. Studying these interactions, researchers are developing drugs to treat many different neurological disorders, including pain, neurodegenerative diseases such as Parkinson's disease and Alzheimer's disease, psychological disorders, addiction, and many others.
Neuropsychopharmacology, an interdisciplinary science related to psychopharmacology and fundamental neuroscience, is the study of the neural mechanisms that drugs act upon to influence behavior. It entails research of mechanisms of neuropathology, pharmacodynamics, psychiatric illness, and states of consciousness. These studies are instigated at the detailed level involving neurotransmission/receptor activity, bio-chemical processes, and neural circuitry. Neuropsychopharmacology supersedes psychopharmacology in the areas of "how" and "why", and additionally addresses other issues of brain function. Accordingly, the clinical aspect of the field includes psychiatric (psychoactive) as well as neurologic (non-psychoactive) pharmacology-based treatments. Developments in neuropsychopharmacology may directly impact the studies of anxiety disorders, affective disorders, psychotic disorders, degenerative disorders, eating behavior, and sleep behavior.
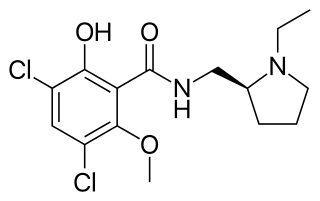
Raclopride is a typical antipsychotic. It acts as a selective antagonist on D2 dopamine receptors. It has been used in trials studying Parkinson Disease.

Nora D. Volkow is a Mexican-American psychiatrist. She is currently the director of the National Institute on Drug Abuse (NIDA), which is part of the National Institutes of Health (NIH).

Altanserin is a compound that binds to the 5-HT2A receptor. Labeled with the isotope fluorine-18 it is used as a radioligand in positron emission tomography (PET) studies of the brain, i.e., studies of the 5-HT2A neuroreceptors. Besides human neuroimaging studies altanserin has also been used in the study of rats.

WAY-100635 is a piperazine drug and research chemical widely used in scientific studies. It was originally believed to act as a selective 5-HT1A receptor antagonist, but subsequent research showed that it also acts as potent full agonist at the D4 receptor. It is sometimes referred to as a silent antagonist at the former receptor. It is closely related to WAY-100135.

Setoperone is a compound that is a ligand to the 5-HT2A receptor. It can be radiolabeled with the radioisotope fluorine-18 and used as a radioligand with positron emission tomography (PET). Several research studies have used the radiolabeled setoperone in neuroimaging for the studying neuropsychiatric disorders, such as depression or schizophrenia.
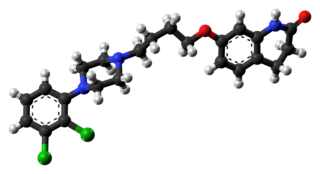
Cariprazine, sold under the brand name Vraylar among others, is an atypical antipsychotic developed by Gedeon Richter, which is used in the treatment of schizophrenia, bipolar mania, bipolar depression, and major depressive disorder. It acts primarily as a D3 and D2 receptor partial agonist, with a preference for the D3 receptor. Cariprazine is also a partial agonist at the serotonin 5-HT1A receptor and acts as an antagonist at 5-HT2B and 5-HT2A receptors, with high selectivity for the D3 receptor. It is taken by mouth.
The causes of schizophrenia that underlie the development of schizophrenia, a psychiatric disorder, are complex and not clearly understood. A number of hypotheses including the dopamine hypothesis, and the glutamate hypothesis have been put forward in an attempt to explain the link between altered brain function and the symptoms and development of schizophrenia.

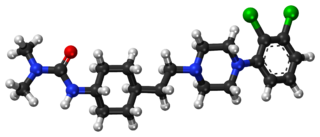
Brexpiprazole, sold under the brand name Rexulti among others, is a medication used for the treatment of major depressive disorder, schizophrenia, and agitation associated with dementia due to Alzheimer's disease. It is an atypical antipsychotic.

Iomazenil is an antagonist and partial inverse agonist of benzodiazepine and a potential treatment for alcohol use disorder. The compound was introduced in 1989 by pharmaceutical company Hoffmann-La Roche as an Iodine-123-labelled SPECT tracer for imaging benzodiazepine receptors in the brain. Iomazenil is an analogue of flumazenil (Ro15-1788).

Hypofrontality is a state of decreased cerebral blood flow (CBF) in the prefrontal cortex of the brain. Hypofrontality is symptomatic of several neurological medical conditions, such as schizophrenia, attention deficit hyperactivity disorder (ADHD), bipolar disorder, and major depressive disorder. This condition was initially described by Ingvar and Franzén in 1974, through the use of xenon blood flow technique with 32 detectors to image the brains of patients with schizophrenia. This finding was confirmed in subsequent studies using the improved spatial resolution of positron emission tomography with the fluorodeoxyglucose (18F-FDG) tracer. Subsequent neuroimaging work has shown that the decreases in prefrontal CBF are localized to the medial, lateral, and orbital portions of the prefrontal cortex. Hypofrontality is thought to contribute to the negative symptoms of schizophrenia.
Dopamine therapy is the regulation of levels of the neurotransmitter dopamine through the use of either agonists, or antagonists; and has been used in the treatment of disorders characterized by a dopamine imbalance. Dopamine replacement therapy (DRT) is an effective treatment for patients with decreased levels of dopamine. Often dopamine antagonists, compounds that activate dopamine receptors in the absence of that receptor's physiological ligand, the neurotransmitter dopamine, are used in this therapy. DRT has been shown to reduce symptoms and increase lifespan for patients with Parkinson's disease. Dopamine regulation plays a critical role in human mental and physical health. The neurons that contain the neurotransmitter are clustered in the midbrain region in an area called the substantia nigra. In Parkinson's patients, the death of dopamine-transmitting neurons in this area leads to abnormal nerve-firing patterns that cause motor problems. Research in patients with schizophrenia indicates abnormalities in dopamine receptor structure and function.
F. Markus Leweke is a German psychiatrist and psychotherapist. He is a professor and Chair in Youth Depression Studies at the Brain and Mind Centre of the University of Sydney, Australia and a work group leader at the Central Institute of Mental Health in Mannheim, Germany.
Anne Lingford-Hughes is a British psychiatrist who is Professor of Addiction Biology at Imperial College London. She works on addictions at the Central and North West London NHS Foundation Trust. Her research uses neuroimaging and pharmacology to understand the neurobiology of addiction.
References
- ↑ "How Dopamine Tunes Working Memory". The Scientist. Retrieved 2018-02-03.
- ↑ "Marijuana use may reduce dopamine in the brain". Medical News Today. Retrieved 2018-02-03.
- ↑ "www.capitalbay.news/news/1020640-heavy-cannabis-use-does-affect-learning-and-memory.html". www.capitalbay.news. Retrieved 2018-02-03.
- ↑ "National Academy of Medicine elects 79 new members". National Academy of Medicine . Retrieved December 10, 2016.