Related Research Articles

Antipsychotics, also known as neuroleptics, are a class of psychotropic medication primarily used to manage psychosis, principally in schizophrenia but also in a range of other psychotic disorders. They are also the mainstay together with mood stabilizers in the treatment of bipolar disorder.

Psychosis is an abnormal condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.
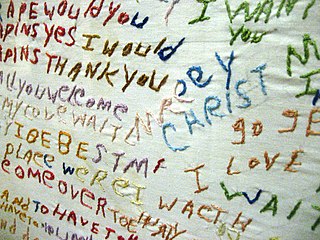
Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations, delusions, and disorganized thinking. Other symptoms include social withdrawal, decreased emotional expression, and apathy. Symptoms typically develop gradually, begin during young adulthood, and in many cases never become resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a history that includes the person's reported experiences, and reports of others familiar with the person. To be diagnosed with schizophrenia, symptoms and functional impairment need to be present for six months (DSM-5) or one month (ICD-11). Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.

Olanzapine is an atypical antipsychotic primarily used to treat schizophrenia and bipolar disorder. For schizophrenia, it can be used for both new-onset disease and long-term maintenance. It is taken by mouth or by injection into a muscle.
The dopamine hypothesis of schizophrenia or the dopamine hypothesis of psychosis is a model that attributes the positive symptoms of schizophrenia to a disturbed and hyperactive dopaminergic signal transduction. The model draws evidence from the observation that a large number of antipsychotics have dopamine-receptor antagonistic effects. The theory, however, does not posit dopamine overabundance as a complete explanation for schizophrenia. Rather, the overactivation of D2 receptors, specifically, is one effect of the global chemical synaptic dysregulation observed in this disorder.
Stimulant psychosis is a mental disorder characterized by psychotic symptoms which involves and typically occurs following an overdose or several day 'binge' on psychostimulants; however, it has also been reported to occur in approximately 0.1% of individuals, within the first several weeks after starting amphetamine or methylphenidate therapy. Methamphetamine psychosis, or long-term effects of stimulant use in the brain, depend upon genetics and may persist for some time.
Dr. Thomas McGlashan is an American professor of psychiatry at Yale University, well known for his academic contributions to the study of schizophrenia and other mental illnesses.
Risk factors of schizophrenia include many genetic and environmental phenomena. The prevailing model of schizophrenia is that of a special neurodevelopmental disorder with no precise boundary or single cause. Schizophrenia is thought to develop from very complex gene–environment interactions with vulnerability factors. The interactions of these risk factors are intricate, as numerous and diverse medical insults from conception to adulthood can be involved. The combination of genetic and environmental factors leads to deficits in the neural circuits that affect sensory input and cognitive functions.
In medicine, a prodrome is an early sign or symptom that often indicates the onset of a disease before more diagnostically specific signs and symptoms develop. It is derived from the Greek word prodromos, meaning "running before". Prodromes may be non-specific symptoms or, in a few instances, may clearly indicate a particular disease, such as the prodromal migraine aura.
Early intervention in psychosis is a clinical approach to those experiencing symptoms of psychosis for the first time. It forms part of a new prevention paradigm for psychiatry and is leading to reform of mental health services, especially in the United Kingdom and Australia.
Barbara A. Cornblatt is Professor of Psychiatry and Molecular Medicine at Hofstra Northwell School of Medicine. She is known for her research on serious mental disorders, with a specific focus on psychosis and schizophrenia. Her efforts to find treatments to help youth with mental illness led to the development of the Recognition and Prevention Program, which she founded in 1998.
Patrick Dennistoun McGorry FAA FASSA FAHMS FRCP FRANZCP is an Irish-born Australian psychiatrist known for his development of the early intervention services for emerging mental disorders in young people.

The prognosis of schizophrenia is varied at the individual level. In general it has great human and economics costs. It results in a decreased life expectancy of 12–15 years primarily due to its association with obesity, little exercise, and smoking, while an increased rate of suicide plays a lesser role. These differences in life expectancy increased between the 1970s and 1990s, and between the 1990s and 2000s. This difference has not substantially changed in Finland for example – where there is a health system with open access to care.
The diagnosis of schizophrenia, a psychotic disorder, is based on criteria in either the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, or the World Health Organization's International Classification of Diseases (ICD). Clinical assessment of schizophrenia is carried out by a mental health professional based on observed behavior, reported experiences, and reports of others familiar with the person. Diagnosis is usually made by a psychiatrist. Associated symptoms occur along a continuum in the population and must reach a certain severity and level of impairment before a diagnosis is made. Schizophrenia has a prevalence rate of 0.3-0.7% in the United States

Schizophrenia affects around 0.3–0.7% of people at some point in their life, or 21 million people worldwide as of 2011. By using precise methods in its diagnosis and a large, representative population, schizophrenia seems to occur with relative consistency over time during the last half-century.

The Kraepelinian dichotomy is the division of the major endogenous psychoses into the disease concepts of dementia praecox, which was reformulated as schizophrenia by Eugen Bleuler by 1908, and manic-depressive psychosis, which has now been reconceived as bipolar disorder. This division was formally introduced in the sixth edition of Emil Kraepelin's psychiatric textbook Psychiatrie. Ein Lehrbuch für Studirende und Aerzte, published in 1899. It has been highly influential on modern psychiatric classification systems, the DSM-IV-TR and ICD-10, and is reflected in the taxonomic separation of schizophrenia from affective psychosis. However, there is also a diagnosis of schizoaffective disorder to cover cases that seem to show symptoms of both.
Sex differences in schizophrenia are widely reported. Men and women exhibit different rates of incidence and prevalence, age at onset, symptom expression, course of illness, and response to treatment. Reviews of the literature suggest that understanding the implications of sex differences on schizophrenia may help inform individualized treatment and positively affect outcomes.
A self-disorder, also called ipseity disturbance, is a psychological phenomenon of disruption or diminishing of a person's sense of minimal self-awareness. The sense of minimal self refers to the very basic sense of having experiences that are one's own; it has no properties, unlike the more extended sense of self, the narrative self, which is characterized by the person's reflections on themselves as a person, things they like, their identity, and other aspects that are the result of reflection on one's self. Disturbances in the sense of minimal self, as measured by the Examination of Anomalous Self-Experience (EASE), aggregate in the schizophrenia spectrum disorders, to include schizotypal personality disorder, and distinguish them from other conditions such as psychotic bipolar disorder and borderline personality disorder.

Basic symptoms of schizophrenia are subjective symptoms, described as experienced from a person's perspective, which show evidence of underlying psychopathology. Basic symptoms have generally been applied to the assessment of people who may be at risk to develop psychosis. Though basic symptoms are often disturbing for the person, problems generally do not become evident to others until the person is no longer able to cope with their basic symptoms. Basic symptoms are more specific to identifying people who exhibit signs of prodromal psychosis (prodrome) and are more likely to develop schizophrenia over other disorders related to psychosis. Schizophrenia is a psychotic disorder, but is not synonymous with psychosis. In the prodrome to psychosis, uncharacteristic basic symptoms develop first, followed by more characteristic basic symptoms and brief and self-limited psychotic-like symptoms, and finally the onset of psychosis. People who were assessed to be high risk according to the basic symptoms criteria have a 48.5% likelihood of progressing to psychosis. In 2015, the European Psychiatric Association issued guidance recommending the use of a subscale of basic symptoms, called the Cognitive Disturbances scale (COGDIS), in the assessment of psychosis risk in help-seeking psychiatric patients; in a meta-analysis, COGDIS was shown to be as predictive of transition to psychosis as the Ultra High Risk (UHR) criteria up to 2 years after assessment, and significantly more predictive thereafter. The basic symptoms measured by COGDIS, as well as those measured by another subscale, the Cognitive-Perceptive basic symptoms scale (COPER), are predictive of transition to schizophrenia.
Paolo Fusar-Poli is an Italian medical doctor, psychiatrist, and clinical academic researcher at the Institute of Psychiatry, Psychology and Neuroscience, King's College, London and at the Department of Brain and Behavioral Sciences, University of Pavia.
References
- ↑ Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC, Rakkar A (1996). "Monitoring and care of young people at incipient risk of psychosis". Schizophr Bull. 22 (2): 283–303. doi: 10.1093/schbul/22.2.283 . PMID 8782287.
- ↑ "ORYGEN Youth Health". Archived from the original on 2009-10-24. Retrieved 2011-08-04.
- ↑ Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC, Rakkar A (1996). "Monitoring and care of young people at incipient risk of psychosis". Schizophr Bull. 22 (2): 283–303. doi: 10.1093/schbul/22.2.283 . PMID 8782287.
- ↑ Broome MR, Woolley JB, Johns LC, et al. (August 2005). "Outreach and support in south London (OASIS): implementation of a clinical service for prodromal psychosis and the at risk mental state". Eur. Psychiatry. 20 (5–6): 372–8. doi:10.1016/j.eurpsy.2005.03.001. PMID 16171652. S2CID 27207646.
- ↑ PRIME
- ↑ (COPE)
- ↑ "Emory University". Archived from the original on 2011-07-22. Retrieved 2011-08-04.
- ↑ Yung AR, Phillips LJ, Yuen HP, et al. (March 2003). "Psychosis prediction: 12-month follow up of a high-risk ("prodromal") group". Schizophr. Res. 60 (1): 21–32. doi:10.1016/S0920-9964(02)00167-6. PMID 12505135. S2CID 31342026.
- ↑ McGorry PD, Yung AR, Phillips LJ, et al. (October 2002). "Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms". Arch. Gen. Psychiatry. 59 (10): 921–8. doi: 10.1001/archpsyc.59.10.921 . PMID 12365879.
- ↑ Morrison AP, French P, Parker S, et al. (May 2007). "Three-year follow-up of a randomized controlled trial of cognitive therapy for the prevention of psychosis in people at ultrahigh risk". Schizophr Bull. 33 (3): 682–7. doi:10.1093/schbul/sbl042. PMC 2526150 . PMID 16973786.
- ↑ Schäfer Amminger; Papageorgiou Harrigan; Cotton McGorry, Berger (2008). "Indicated Prevention of Psychotic Disorders with Long-Chainomega-3 Fatty Acids: A Randomized, Placebo-Controlled Trial". Schizophrenia Research. 102 (1–3): 252. doi:10.1016/s0920-9964(08)70758-8. S2CID 53301111.
- ↑ Yung AR, Yuen HP, McGorry PD, et al. (2005). "Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States". Aust N Z J Psychiatry. 39 (11–12): 964–71. doi:10.1080/j.1440-1614.2005.01714.x. PMID 16343296. S2CID 145477493.