Related Research Articles

A febrile seizure, also known as a fever fit or febrile convulsion, is a seizure associated with a high body temperature but without any serious underlying health issue. They most commonly occur in children between the ages of 6 months and 5 years. Most seizures are less than five minutes in duration, and the child is completely back to normal within an hour of the event. There are two types: simple febrile seizures and complex febrile seizures. Simple febrile seizures involve an otherwise healthy child who has at most one tonic-clonic seizure lasting less than 15 minutes in a 24-hour period. Complex febrile seizures have focal symptoms, last longer than 15 minutes, or occur more than once within 24 hours. About 80% are classified as simple febrile seizures.
Absence seizures are one of several kinds of generalized seizures. In the past, absence epilepsy was referred to as "pyknolepsy," a term derived from the Greek word "pyknos," signifying "extremely frequent" or "grouped". These seizures are sometimes referred to as petit mal seizures ; however, usage of this terminology is no longer recommended. Absence seizures are characterized by a brief loss and return of consciousness, generally not followed by a period of lethargy. Absence seizures are most common in children. They affect both sides of the brain.
A headache is often present in patients with epilepsy. If the headache occurs in the vicinity of a seizure, it is defined as peri-ictal headache, which can occur either before (pre-ictal) or after (post-ictal) the seizure, to which the term ictal refers. An ictal headache itself may or may not be an epileptic manifestation. In the first case it is defined as ictal epileptic headache or simply epileptic headache. It is a real painful seizure, that can remain isolated or be followed by other manifestations of the seizure. On the other hand, the ictal non-epileptic headache is a headache that occurs during a seizure but it is not due to an epileptic mechanism. When the headache does not occur in the vicinity of a seizure it is defined as inter-ictal headache. In this case it is a disorder autonomous from epilepsy, that is a comorbidity.

Central hypoventilation syndrome (CHS) is a sleep-related breathing disorder that causes ineffective breathing, apnea, or respiratory arrest during sleep. CHS can either be congenital (CCHS) or acquired (ACHS) later in life. The condition can be fatal if untreated. CCHS was once known as Ondine's curse.
Landau–Kleffner syndrome (LKS)—also called infantile acquired aphasia, acquired epileptic aphasia or aphasia with convulsive disorder—is a rare childhood neurological syndrome.
Non-epileptic seizures (NES), also known as non-epileptic events, are paroxysmal events that appear similar to an epileptic seizure but do not involve abnormal, rhythmic discharges of neurons in the brain. Symptoms may include shaking, loss of consciousness, and loss of bladder control.
Hopkins syndrome is a neurological disorder. Its cause has not been established, but its association with asthma exacerbations has led to suspicion that the initial viral insult that causes the respiratory infection is also implicated in the subsequent paralysis. Herpes simplex virus type I DNA has been found in the cerebrospinal fluid of at least one patient diagnosed with Hopkins syndrome. In several cases, anti-viral antibody titers for echovirus, enterovirus, coxsackievirus and poliovirus types 1, 2 and 3 were specifically sought; all were negative., There is one reported case in which Mycoplasma pneumoniae infection was found in the patient.
The postictal state is the altered state of consciousness after an epileptic seizure. It usually lasts between 5 and 30 minutes, but sometimes longer in the case of larger or more severe seizures, and is characterized by drowsiness, confusion, nausea, hypertension, headache or migraine, and other disorienting symptoms.
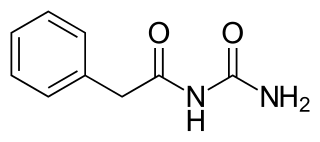
Phenacemide, also known as phenylacetylurea, is an anticonvulsant of the ureide (acetylurea) class. It is a congener and ring-opened analogue of phenytoin, and is structurally related to the barbiturates and to other hydantoins. Phenacemide was introduced in 1949 for the treatment of epilepsy, but was eventually withdrawn due to toxicity.
Todd's paresis is focal weakness in a part or all of the body after a seizure. This weakness typically affects the limbs and is localized to either the left or right side of the body. It usually subsides completely within 48 hours. Todd's paresis may also affect speech, eye position (gaze), or vision.
Reflex asystolic syncope (RAS) is a form of syncope encountered mainly, but not exclusively, in young children. Reflex anoxic seizures are not epileptic seizures or epilepsy. This is usually a consequence of a reduction in cerebral perfusion by oxygenated blood. It can be a result of either a sudden reduction in the blood flow to the brain, a drop in the oxygen content of the blood supplying the brain, or a combination of the two. Syncope can have different meanings ranging from transient loss of consciousness, usually accompanied by a decrease or loss in postural tone, to tonic and myoclonic events and nonepileptic spasms.

A generalized tonic–clonic seizure, commonly known as a grand mal seizure or GTCS, is a type of generalized seizure that produces bilateral, convulsive tonic and clonic muscle contractions. Tonic–clonic seizures are the seizure type most commonly associated with epilepsy and seizures in general and the most common seizure associated with metabolic imbalances. It is a misconception that they are the sole type of seizure, as they are the main seizure type in approximately 10% of those with epilepsy.

Benign Rolandic epilepsy or self-limited epilepsy with centrotemporal spikes is the most common epilepsy syndrome in childhood. Most children will outgrow the syndrome, hence the label benign. The seizures, sometimes referred to as sylvian seizures, start around the central sulcus of the brain.
Panayiotopoulos syndrome is a common idiopathic childhood-related seizure disorder that occurs exclusively in otherwise normal children and manifests mainly with autonomic epileptic seizures and autonomic status epilepticus. An expert consensus has defined Panayiotopoulos syndrome as "a benign age-related focal seizure disorder occurring in early and mid-childhood. It is characterized by seizures, often prolonged, with predominantly autonomic symptoms, and by an EEG [electroencephalogram] that shows shifting and/or multiple foci, often with occipital predominance."

Schimmelpenning syndrome is a neurocutaneous condition characterized by one or more sebaceous nevi, usually appearing on the face or scalp, associated with anomalies of the central nervous system, ocular system, skeletal system, cardiovascular system and genitourinary system.
Diffuse myelinoclastic sclerosis, sometimes referred to as Schilder's disease, is a very infrequent neurodegenerative disease that presents clinically as pseudotumoural demyelinating lesions, making its diagnosis difficult. It usually begins in childhood, affecting children between 5 and 14 years old, but cases in adults are also possible.
Migralepsy is a rare condition in which a migraine is followed, within an hour period, by an epileptic seizure. Because of the similarities in signs, symptoms, and treatments of both conditions, such as the neurological basis, the psychological issues, and the autonomic distress that is created from them, they individually increase the likelihood of causing the other. However, also because of the sameness, they are often misdiagnosed for each other, as migralepsy rarely occurs.

Tuber cinereum hamartoma is a benign tumor in which a disorganized collection of neurons and glia accumulate at the tuber cinereum of the hypothalamus on the floor of the third ventricle. It is a congenital malformation, included on the spectrum of gray matter heterotopias. Formation occurs during embryogenesis, typically between days 33 and 41 of gestation. Size of the tumor varies from one to three centimeters in diameter, with the mean being closer to the low end of this range. It is estimated to occur at a frequency of one in one million individuals.

Epilepsy is a neurological condition of recurrent episodes of unprovoked epileptic seizures. A seizure is an abnormal neuronal brain activity that can cause intellectual, emotional, and social consequences. Epilepsy affects children and adults of all ages and races, it is one of the most common neurological disorders of the nervous system. As well as, this condition is more common among children than adults affecting about 6 out of 1000 US children that are between the age of 0 to 5 years old. The epileptic seizures can be of different types depending on the part of the brain that was affected, seizures are classified in 2 main types partial seizure or genralized seizure.
Elaine Wyllie is a professor of neurology at the Cleveland Clinic Lerner College of Medicine and staff physician in Cleveland Clinic’s Epilepsy Center. Her research focuses on the role of epilepsy surgery in children with drug-resistant seizures.
References
- ↑ Leung, Alexander K.C.; Leung, Amy A.M.; Wong, Alex H.C.; Hon, Kam Lun (2019). "Breath-Holding Spells in Pediatrics: A Narrative Review of the Current Evidence". Current Pediatric Reviews. 15 (1): 22–29. doi:10.2174/1573396314666181113094047. ISSN 1573-3963. PMC 6696822 . PMID 30421679.
- 1 2 Flodine, Tierney E.; Mendez, Magda D. (2022), "Breath Holding Spells", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30969604 , retrieved 2022-11-23
- ↑ Fujisawa, Hironori; Yoshida, Yuya; Niida, Yo; Hasegawa, Mitsuhiro; Yamashita, Junkoh (2005). "Cyanotic breath-holding spell: a life-threatening complication after radical resection of a cervicomedullary ganglioglioma". Pediatric Neurosurgery. 41 (2): 93–97. doi:10.1159/000085163. ISSN 1016-2291. PMID 15942280. S2CID 1196104.
- ↑ Goldman, Ran D. (2008). "Breath-holding spells in infants". Canadian Family Physician. 61 (2): 149–150. doi: 10.4103/0019-5545.43635 . ISSN 1715-5258. PMC 4325862 . PMID 25676645.
- ↑ Breningstall, G. N. (1996-02-01). "Breath-holding spells". Pediatric Neurology. 14 (2): 91–97. doi:10.1016/0887-8994(96)00006-9. ISSN 0887-8994. PMID 8703234.
- ↑ Subbarayan, A.; Ganesan, B.; Anbumani; Jayanthini (2008). "Temperamental traits of breath holding children: A case control study". Indian Journal of Psychiatry. 50 (3): 192–196. doi: 10.4103/0019-5545.43635 . ISSN 0019-5545. PMC 2738355 . PMID 19742234.
- ↑ Poets CF, Samuels MP, Wardrop CA, Picton-Jones E, Southall DP (April 1992). "Reduced haemoglobin levels in infants presenting with apparent life-threatening events--a retrospective investigation". Acta Paediatr. 81 (4): 319–21. doi:10.1111/j.1651-2227.1992.tb12234.x. PMID 1606392. S2CID 33298390.
- ↑ Colina KF, Abelson HT (March 1995). "Resolution of breath-holding spells with treatment of concomitant anemia". J. Pediatr. 126 (3): 395–7. doi:10.1016/S0022-3476(95)70456-6. PMID 7869200.
- ↑ Donma MM (January 1998). "Clinical efficacy of piracetam in treatment of breath-holding spells". Pediatr. Neurol. 18 (1): 41–5. doi:10.1016/S0887-8994(97)00153-7. PMID 9492090.
- ↑ Azam M, Bhatti N, Shahab N (2008). "Piracetam in severe breath holding spells". Int J Psychiatry Med. 38 (2): 195–201. doi:10.2190/PM.38.2.f. PMID 18724570. S2CID 36114201.
- ↑ DiMario FJ (January 1992). "Breath-holding spells in childhood". Am. J. Dis. Child. 146 (1): 125–31. doi:10.1001/archpedi.1992.02160130127035. PMID 1736640.
- 1 2 Breningstall GN (February 1996). "Breath-holding spells". Pediatr. Neurol. 14 (2): 91–7. doi:10.1016/0887-8994(96)00006-9. PMID 8703234.
- ↑ Allan WC, Gospe SM (March 2005). "Seizures, syncope, or breath-holding presenting to the pediatric neurologist--when is the etiology a life-threatening arrhythmia?". Semin Pediatr Neurol. 12 (1): 2–9. doi:10.1016/j.spen.2004.11.004. PMID 15929459.