Related Research Articles

Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where they help keep the bite area unclotted long enough for the animal to obtain some blood. As a class of medications, anticoagulants are used in therapy for thrombotic disorders. Oral anticoagulants (OACs) are taken by many people in pill or tablet form, and various intravenous anticoagulant dosage forms are used in hospitals. Some anticoagulants are used in medical equipment, such as sample tubes, blood transfusion bags, heart–lung machines, and dialysis equipment. One of the first anticoagulants, warfarin, was initially approved as a rodenticide.

Warfarin is an anticoagulant used as a medication under several brand names including Coumadin. While the drug is described as a "blood thinner", it does not reduce viscosity but rather inhibits coagulation. Accordingly, it is commonly used to prevent blood clots in the circulatory system such as deep vein thrombosis and pulmonary embolism, and to protect against stroke in people who have atrial fibrillation, valvular heart disease, or artificial heart valves. Less commonly, it is used following ST-segment elevation myocardial infarction and orthopedic surgery. It is usually taken by mouth, but may also be administered intravenously.

Cardiopulmonary bypass (CPB) is a technique in which a machine temporarily takes over the function of the heart and lungs during cardiac surgery, maintaining the circulation of blood and oxygen to the body. The CPB pump itself is often referred to as a heart-lung machine or "the pump". Cardiopulmonary bypass pumps are operated by perfusionists. CPB is a form of extracorporeal circulation. Extracorporeal membrane oxygenation (ECMO) is generally used for longer-term treatment.

Extracorporeal membrane oxygenation (ECMO), also known as extracorporeal life support (ECLS), is an extracorporeal technique of providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of oxygen, gas exchange or blood supply (perfusion) to sustain life. The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation. The device used is a membrane oxygenator, also known as an artificial lung.

Heparin-induced thrombocytopenia (HIT) is the development of thrombocytopenia, due to the administration of various forms of heparin, an anticoagulant. HIT predisposes to thrombosis. When thrombosis is identified the condition is called heparin-induced thrombocytopenia and thrombosis (HITT). HIT is caused by the formation of abnormal antibodies that activate platelets, which release microparticles that activate thrombin, leading to thrombosis. If someone receiving heparin develops new or worsening thrombosis, or if the platelet count falls, HIT can be confirmed with specific blood tests.

Cardiogenic shock is a medical emergency resulting from inadequate blood flow to the body's organs due to the dysfunction of the heart. Signs of inadequate blood flow include low urine production, cool arms and legs, and decreased level of consciousness. People may also have a severely low blood pressure and heart rate.
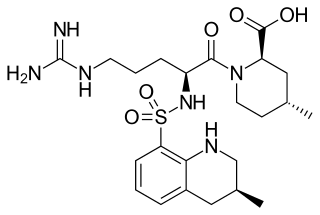
Argatroban is an anticoagulant that is a small molecule direct thrombin inhibitor. In 2000, argatroban was licensed by the Food and Drug Administration (FDA) for prophylaxis or treatment of thrombosis in patients with heparin-induced thrombocytopenia (HIT). In 2002, it was approved for use during percutaneous coronary interventions in patients who have HIT or are at risk for developing it. In 2012, it was approved by the MHRA in the UK for anticoagulation in patients with heparin-induced thrombocytopenia Type II (HIT) who require parenteral antithrombotic therapy.

Warfarin-induced skin necrosis is a condition in which skin and subcutaneous tissue necrosis occurs due to acquired protein C deficiency following treatment with anti-vitamin K anticoagulants.

Phenprocoumon is a long-acting blood thinner drug to be taken by mouth, and a derivative of coumarin. It acts as a vitamin K antagonist and inhibits blood clotting (coagulation) by blocking synthesis of coagulation factors II, VII, IX and X. It is used for the prophylaxis and treatment of thromboembolic disorders such as heart attacks and pulmonary (lung) embolism. The most common adverse effect is bleeding. The drug interacts with a large number of other medications, including aspirin and St John's Wort. It is the standard coumarin used in Germany, Austria, and other European countries.
Abiomed, Inc. is a medical device technology company that operates as a stand-alone business within Johnson & Johnson's MedTech Segment. Abiomed develops and manufactures temporary external and implantable mechanical circulatory support devices. The company is headquartered in Danvers, Massachusetts with additional offices in Woburn, Baltimore, Berlin, Aachen, and Tokyo.
Prothrombin complex concentrate (PCC), also known as factor IX complex, sold under the brand name Kcentra among others, is a combination medication made up of blood clotting factors II, IX, and X. Some versions also contain factor VII. It is used to treat and prevent bleeding in hemophilia B if pure factor IX is not available. It may also be used for reversal of warfarin therapy. It is given by slow injection into a vein.
Direct factor Xa inhibitors (xabans) are anticoagulants, used to both treat and prevent blood clots in veins, and prevent stroke and embolism in people with atrial fibrillation (AF).

Left atrial appendage occlusion (LAAO), also referred to as left atrial appendage closure (LAAC), is a procedure used to reduce the risk of blood clots from the left atrial appendage entering the bloodstream and causing a stroke in those with non-valvular atrial fibrillation.
Destination therapy is a therapy that is final rather than being a transitional stage until another therapy—thus, in transportation metaphor, a destination in itself rather than merely a bridge or road to the destination. The term usually refers to ventricular assist devices or mechanical circulatory support to keep the existing heart going, not just until a heart transplant can occur, but for the rest of the patient's life expectancy. It is thus a course of treatment for severe heart failure patients who are not likely candidates for transplant. In contrast, bridge-to-transplant therapy is a way to stay alive long enough, and stay healthy enough, to await transplant while maintaining eligibility for transplant.
The management of atrial fibrillation (AF) is focused on preventing temporary circulatory instability, stroke and other ischemic events. Control of heart rate and rhythm are principally used to achieve the former, while anticoagulation may be employed to decrease the risk of stroke. Within the context of stroke, the discipline may be referred to as stroke prevention in atrial fibrillation (SPAF). In emergencies, when circulatory collapse is imminent due to uncontrolled rapid heart rate, immediate cardioversion may be indicated.
Thoratec Corporation is a United States-based company that develops, manufactures, and markets proprietary medical devices used for mechanical circulatory support for the treatment of heart-failure patients worldwide. It is a global leader in mechanical circulatory support devices, particularly in ventricular assist devices (VADs).

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), which involves coronary angioplasty. The angioplasty uses the insertion of a balloon and/or stents to open up the artery. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.
Impella is a family of medical devices used for temporary ventricular support in patients with depressed heart function. Some versions of the device can provide left heart support during other forms of mechanical circulatory support including ECMO and Centrimag.
Pump thrombosis (PT) is considered a specific case of a major device malfunction, and is classified as either suspected or confirmed pump thrombus. Typically, the device is an implanted blood pump such as a left ventricular assist device. The malfunction is a blockage in the flow of blood anywhere along a vessel and it is mainly due to the bio-incompatible presence of a fairly complex mechanical apparatus. Pump thrombus is dreaded complication of CF LVAD technology that can require repeat surgery to replace the pump or lead to death.
References
- ↑ Nakagawa, S; et al. (2017), "Palliative care interventions before left ventricular assist device implantation in both bridge to transplant and destination therapy", J Palliat Med, 20 (9): 977–983, doi:10.1089/jpm.2016.0568, PMID 28504892.
- ↑ Prasad, MA; Kulik, LM (2014), "The role of bridge therapy prior to orthotopic liver transplantation", J Natl Compr Canc Netw, 12 (8): 1183–1190, quiz 1191, doi: 10.6004/jnccn.2014.0113 , PMID 25099448.
- ↑ Cordova, FC; Criner, GJ (2002), "Lung volume reduction surgery as a bridge to lung transplantation", Am J Respir Med, 1 (5): 313–324, doi: 10.1007/BF03256625 , PMID 14720034, S2CID 30037357.
- ↑ Shigemura, N; et al. (2013), "Lung transplantation after lung volume reduction surgery", Transplantation, 96 (4): 421–425, doi: 10.1097/TP.0b013e31829853ac , PMID 23736352, S2CID 46364233.
- ↑ Bull, DA; Reid, BB; Selzman, CH; Mesley, R; Drakos, S; Clayson, S; Stoddard, G; Gilbert, E; Stehlik, J; Bader, F; Kfoury, A; Budge, D; Eckels, DD; Fuller, A; Renlund, D; Patel, AN (July 2010). "The impact of bridge-to-transplant ventricular assist device support on survival after cardiac transplantation". The Journal of Thoracic and Cardiovascular Surgery. 140 (1): 169–73. doi:10.1016/j.jtcvs.2010.03.026. PMID 20451930.
- ↑ Sef, D; Mohite, P; De Robertis, F; Verzelloni Sef, A; Mahesh, B; Stock, U; Simon, A (September 2020). "Bridge to heart transplantation using the Levitronix CentriMag short-term ventricular assist device". Artificial Organs. 44 (9): 1006–1008. doi:10.1111/aor.13709. PMID 32367538. S2CID 218506853.
- ↑ Sef, D; Verzelloni Sef, A; Trkulja, V; Raj, B; Lees, NJ; Walker, C; Mitchell, J; Petrou, M; De Robertis, F; Stock, U; McGovern, I (April 2022). "Midterm outcomes of venovenous extracorporeal membrane oxygenation as a bridge to lung transplantation: Comparison with nonbridged recipients". Journal of Cardiac Surgery. 37 (4): 747–759. doi:10.1111/jocs.16253. PMID 35060184.
- ↑ Wallinder, A; Pellegrino, V; Fraser, JF; McGiffin, DC (2017), "ECMO as a bridge to non-transplant cardiac surgery", J Card Surg, 32 (8): 514–521, doi: 10.1111/jocs.13172 , PMID 28672423, S2CID 3461110.
- ↑ Zaliznyak, M; Stern, L; Cole, R; Shen, A; Nishihara, K; Runyan, C; Fishman, A; Olanisa, L; Olman, M; Singer-Englar, T; Luong, E; Cheng, S; Moriguchi, J; Kobashigawa, J; Esmailian, F; Kittleson, MM (1 April 2022). "Mechanical Circulatory Support as a Bridge-to-Transplant Candidacy: When Does It Work?". ASAIO Journal. 68 (4): 499–507. doi:10.1097/MAT.0000000000001500. PMID 34074853.
- ↑ den Uil, CA; et al. (2017), "Short-term mechanical circulatory support as a bridge to durable left ventricular assist device implantation in refractory cardiogenic shock: a systematic review and meta-analysis", Eur J Cardiothorac Surg, 52 (1): 14–25, doi: 10.1093/ejcts/ezx088 , PMID 28472406.
- ↑ Morrison, LK; et al. (2017), "Rescue extracorporeal membrane oxygenation therapy in methamphetamine toxicity", CJEM, 20 (S2): S14–S19, doi: 10.1017/cem.2017.356 , PMID 28758605.
- ↑ Daley, Brian J.; Taylor, Dana; Aycinena Goicolea, Jose Fernando (2016-03-28), Schwer, William A. (ed.), "Perioperative anticoagulation management", Medscape, retrieved 2017-08-11.
- ↑ Baser, Onur; Supina, Dylan; Sengupta, Nishan; Wang, Li (2011), "Anticoagulation bridging therapy patterns in patients undergoing total hip or total knee replacement in a US health plan: real-world observations and implications", Am Health Drug Benefits, 4 (4): 240–248, PMC 4125758 , PMID 25126354.