Arthritis is a term often used to mean any disorder that affects joints. Symptoms generally include joint pain and stiffness. Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints. In some types of arthritis, other organs are also affected. Onset can be gradual or sudden.

Gout is a form of inflammatory arthritis characterized by recurrent attacks of pain in a red, tender, hot, and swollen joint, caused by the deposition of needle-like crystals of uric acid known as monosodium urate crystals. Pain typically comes on rapidly, reaching maximal intensity in less than 12 hours. The joint at the base of the big toe is affected (Podagra) in about half of cases. It may also result in tophi, kidney stones, or kidney damage.
Rheumatology is a branch of medicine devoted to the diagnosis and management of disorders whose common feature is inflammation in the bones, muscles, joints, and internal organs. Rheumatology covers more than 100 different complex diseases, collectively known as rheumatic diseases, which includes many forms of arthritis as well as lupus and Sjögren's syndrome. Doctors who have undergone formal training in rheumatology are called rheumatologists.
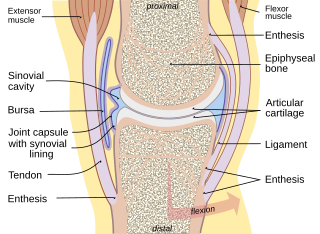
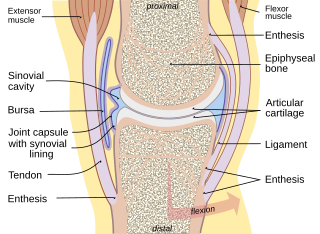
A joint or articulation is the connection made between bones, ossicles, or other hard structures in the body which link an animal's skeletal system into a functional whole. They are constructed to allow for different degrees and types of movement. Some joints, such as the knee, elbow, and shoulder, are self-lubricating, almost frictionless, and are able to withstand compression and maintain heavy loads while still executing smooth and precise movements. Other joints such as sutures between the bones of the skull permit very little movement in order to protect the brain and the sense organs. The connection between a tooth and the jawbone is also called a joint, and is described as a fibrous joint known as a gomphosis. Joints are classified both structurally and functionally.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.

Acute septic arthritis, infectious arthritis, suppurative arthritis, pyogenic arthritis, osteomyelitis, or joint infection is the invasion of a joint by an infectious agent resulting in joint inflammation. Generally speaking, symptoms typically include redness, heat and pain in a single joint associated with a decreased ability to move the joint. Onset is usually rapid. Other symptoms may include fever, weakness and headache. Occasionally, more than one joint may be involved, especially in neonates, younger children and immunocompromised individuals. In neonates, infants during the first year of life, and toddlers, the signs and symptoms of septic arthritis can be deceptive and mimic other infectious and non-infectious disorders.

Rheumatism or rheumatic disorders are conditions causing chronic, often intermittent pain affecting the joints or connective tissue. Rheumatism does not designate any specific disorder, but covers at least 200 different conditions, including arthritis and "non-articular rheumatism", also known as "regional pain syndrome" or "soft tissue rheumatism". There is a close overlap between the term soft tissue disorder and rheumatism. Sometimes the term "soft tissue rheumatic disorders" is used to describe these conditions.
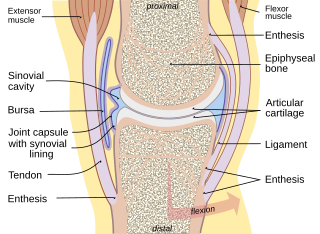
Synovial fluid, also called synovia,[help 1] is a viscous, non-Newtonian fluid found in the cavities of synovial joints. With its egg white–like consistency, the principal role of synovial fluid is to reduce friction between the articular cartilage of synovial joints during movement. Synovial fluid is a small component of the transcellular fluid component of extracellular fluid.

Hyaline cartilage is the glass-like (hyaline) and translucent cartilage found on many joint surfaces. It is also most commonly found in the ribs, nose, larynx, and trachea. Hyaline cartilage is pearl-gray in color, with a firm consistency and has a considerable amount of collagen. It contains no nerves or blood vessels, and its structure is relatively simple.

A tophus is a deposit of monosodium urate crystals, in people with longstanding high levels of uric acid (urate) in the blood, a condition known as hyperuricemia. Tophi are pathognomonic for the disease gout. Most people with tophi have had previous attacks of acute arthritis, eventually leading to the formation of tophi. Chronic tophaceous gout is known as Harrison Syndrome.

Monoarthritis, or monoarticular arthritis, is inflammation (arthritis) of one joint at a time. It is usually caused by trauma, infection, or crystalline arthritis.

An arthropathy is a disease of a joint.

Synovitis is the medical term for inflammation of the synovial membrane. This membrane lines joints that possess cavities, known as synovial joints. The condition is usually painful, particularly when the joint is moved. The joint usually swells due to synovial fluid collection.
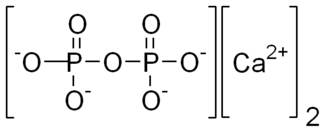
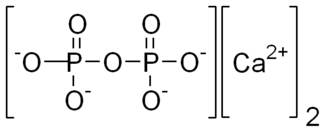
Calcium pyrophosphate (Ca2P2O7) is a chemical compound, an insoluble calcium salt containing the pyrophosphate anion. There are a number of forms reported: an anhydrous form, a dihydrate, Ca2P2O7·2H2O and a tetrahydrate, Ca2P2O7·4H2O. Deposition of dihydrate crystals in cartilage are responsible for the severe joint pain in cases of calcium pyrophosphate deposition disease (pseudo gout) whose symptoms are similar to those of gout. Ca2P2O7 is commonly used as a mild abrasive agent in toothpastes, because of its insolubility and nonreactivity toward fluoride.

Knee effusion, informally known as water on the knee, occurs when excess synovial fluid accumulates in or around the knee joint. It has many common causes, including arthritis, injury to the ligaments or meniscus, or fluid collecting in the bursa, a condition known as prepatellar bursitis.
Arthrocentesis, or joint aspiration, is the clinical procedure performed to diagnose and, in some cases, treat musculoskeletal conditions. The procedure entails using a syringe to collect synovial fluid from or inject medication into the joint capsule. Laboratory analysis of synovial fluid can further help characterize the diseased joint and distinguish between gout, arthritis, and synovial infections such as septic arthritis.
Crystal arthropathy is a class of joint disorder that is characterized by accumulation of tiny crystals in one or more joints. Polarizing microscopy and application of other crystallographic techniques have improved identification of different microcrystals including monosodium urate, calcium pyrophosphate dihydrate, calcium hydroxyapatite, and calcium oxalate.
Milwaukee shoulder syndrome (MSS) (apatite-associated destructive arthritis/Basic calcium phosphate (BCP) crystal arthritis/rapid destructive arthritis of the shoulder is a rare rheumatological condition similar to pseudogout, associated with periarticular or intra-articular deposition of hydroxyapatite or basic calcium phosphate (BCP) crystals. While primarily associated with the shoulder joint, it can affect any joint in the body below the head. Along with symptomatology, the disease typically presents with positive radiologic findings, often showing marked erosion of the humeral head, cartilage, capsule, and bursae. Though rare, it is most often seen in females beginning in their 50s or 60s. Patients often have a history of joint trauma or overuse, calcium pyrophosphate dehydrate crystal deposition, neuroarthropathy, dialysis-related arthropathy or denervation.

Pain in the hip is the experience of pain in the muscles or joints in the hip/ pelvic region, a condition commonly arising from any of a number of factors. Sometimes it is closely associated with lower back pain.

Chondrocalcinosis or cartilage calcification is calcification in hyaline cartilage and/or fibrocartilage. Chondrocalcinosis is an observation that can be visualized through diagnostic imaging tests such as X-rays, CT, MRI, and ultrasound.