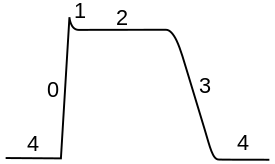
The cardiac action potential is a brief change in voltage across the cell membrane of heart cells. This is caused by the movement of charged atoms between the inside and outside of the cell, through proteins called ion channels. The cardiac action potential differs from action potentials found in other types of electrically excitable cells, such as nerves. Action potentials also vary within the heart; this is due to the presence of different ion channels in different cells.

In neuroscience, repolarization refers to the change in membrane potential that returns it to a negative value just after the depolarization phase of an action potential which has changed the membrane potential to a positive value. The repolarization phase usually returns the membrane potential back to the resting membrane potential. The efflux of potassium (K+) ions results in the falling phase of an action potential. The ions pass through the selectivity filter of the K+ channel pore.
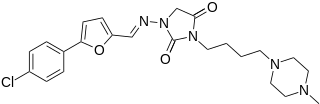
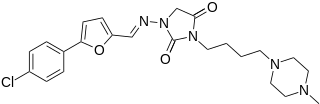
Azimilide is a class ΙΙΙ antiarrhythmic drug. The agents from this heterogeneous group have an effect on the repolarization, they prolong the duration of the action potential and the refractory period. Also they slow down the spontaneous discharge frequency of automatic pacemakers by depressing the slope of diastolic depolarization. They shift the threshold towards zero or hyperpolarize the membrane potential. Although each agent has its own properties and will have thus a different function.

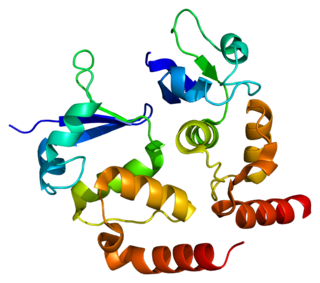
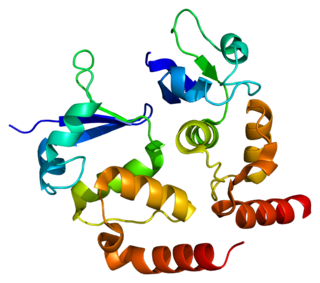
Voltage-gated potassium channels (VGKCs) are transmembrane channels specific for potassium and sensitive to voltage changes in the cell's membrane potential. During action potentials, they play a crucial role in returning the depolarized cell to a resting state.
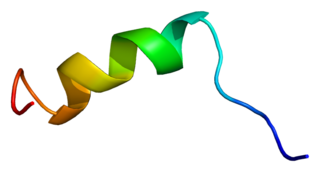
Sodium channel protein type 5 subunit alpha, also known as NaV1.5 is an integral membrane protein and tetrodotoxin-resistant voltage-gated sodium channel subunit. NaV1.5 is found primarily in cardiac muscle, where it mediates the fast influx of Na+-ions (INa) across the cell membrane, resulting in the fast depolarization phase of the cardiac action potential. As such, it plays a major role in impulse propagation through the heart. A vast number of cardiac diseases is associated with mutations in NaV1.5 (see paragraph genetics). SCN5A is the gene that encodes the cardiac sodium channel NaV1.5.

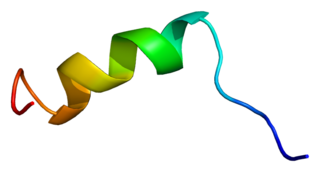
Potassium voltage-gated channel subfamily E member 1 is a protein that in humans is encoded by the KCNE1 gene.

Potassium voltage-gated channel subfamily E member 2 (KCNE2), also known as MinK-related peptide 1 (MiRP1), is a protein that in humans is encoded by the KCNE2 gene on chromosome 21. MiRP1 is a voltage-gated potassium channel accessory subunit associated with Long QT syndrome. It is ubiquitously expressed in many tissues and cell types. Because of this and its ability to regulate multiple different ion channels, KCNE2 exerts considerable influence on a number of cell types and tissues. Human KCNE2 is a member of the five-strong family of human KCNE genes. KCNE proteins contain a single membrane-spanning region, extracellular N-terminal and intracellular C-terminal. KCNE proteins have been widely studied for their roles in the heart and in genetic predisposition to inherited cardiac arrhythmias. The KCNE2 gene also contains one of 27 SNPs associated with increased risk of coronary artery disease. More recently, roles for KCNE proteins in a variety of non-cardiac tissues have also been explored.

Potassium voltage-gated channel, shaker-related subfamily, member 5, also known as KCNA5 or Kv1.5, is a protein that in humans is encoded by the KCNA5 gene.

Potassium voltage-gated channel subfamily D member 2 is a protein that in humans is encoded by the KCND2 gene. It contributes to the cardiac transient outward potassium current (Ito1), the main contributing current to the repolarizing phase 1 of the cardiac action potential.

Potassium voltage-gated channel, Isk-related family, member 3 (KCNE3), also known as MinK-related peptide 2(MiRP2) is a protein that in humans is encoded by the KCNE3 gene.
Potassium voltage-gated channel subfamily D member 3 also known as Kv4.3 is a protein that in humans is encoded by the KCND3 gene. It contributes to the cardiac transient outward potassium current (Ito1), the main contributing current to the repolarizing phase 1 of the cardiac action potential.

Potassium voltage-gated channel subfamily E member 4, originally named MinK-related peptide 3 or MiRP3 when it was discovered, is a protein that in humans is encoded by the KCNE4 gene.

Tedisamil (3,7-dicyclopropylmethyl-9,9-tetramethylene-3,7-diazabicyclo-3,3,1-nonane) is an experimental class III antiarrhythmic agent currently being investigated for the treatment of atrial fibrillation. Tedisamil blocks multiple types of potassium channels in the heart resulting in slowed heart rate. While the effects of tedisamil have been demonstrated in both atrial and ventricular muscle, repolarization is prolonged more efficiently in the atria. Tedisamil is administered intravenously and has a half-life of approximately 8 –13 hours in circulation. Tedisamil is being developed as an alternative to other antiarrhythmics as incidence of additional arrhythmic events is lower compared to other class III agents. Tedisamil also has significant anti-ischemic properties and was initially investigated as a potential treatment for angina until its antiarrhythmic effects were discovered. Tedisamil is manufactured by Solvay Pharmaceuticals Inc. under the proposed trade name Pulzium.

Potassium voltage-gated channel subfamily A member 7 also known as Kv1.7 is a protein that in humans is encoded by the KCNA7 gene. The protein encoded by this gene is a voltage-gated potassium channel subunit. It may contribute to the cardiac transient outward potassium current (Ito1), the main contributing current to the repolarizing phase 1 of the cardiac action potential.

KCNE1-like also known as KCNE1L is a protein that in humans is encoded by the KCNE1L gene.

Celivarone is an experimental drug being tested for use in pharmacological antiarrhythmic therapy. Cardiac arrhythmia is any abnormality in the electrical activity of the heart. Arrhythmias range from mild to severe, sometimes causing symptoms like palpitations, dizziness, fainting, and even death. They can manifest as slow (bradycardia) or fast (tachycardia) heart rate, and may have a regular or irregular rhythm.
N-(p-Amylcinnamoyl)anthranilic acid (ACA) is a modulator of various ion channels in the heart. ACA is an effective reversible inhibitor of calcium-activated chloride channels and, to a lesser extent, cAMP-activated chloride channels, without affecting L-type calcium channels. Calcium-activated chloride channels are believed to be involved in developing arrhythmia.

Budiodarone (ATI-2042) is an antiarrhythmic agent and chemical analog of amiodarone that is currently being studied in clinical trials. Amiodarone is considered the most effective antiarrhythmic drug available, but its adverse side effects, including hepatic, pulmonary and thyroid toxicity as well as multiple drug interactions, are discouraging its use. Budiodarone only differs in structure from amiodarone through the presence of a sec-butyl acetate side chain at position 2 of the benzofuran moiety. This side chain allows for budiodarone to have a shorter half-life in the body than amiodarone which allows it to have a faster onset of action and metabolism while still maintaining similar electrophysiological activity. The faster metabolism of budiodarone allows for fewer adverse side effects than amiodarone principally due to decreased levels of toxicity in the body.

AZD1305 is an experimental drug candidate that is under investigation for the management and reversal of cardiac arrhythmias, specifically atrial fibrillation and flutter. In vitro studies have shown that this combined-ion channel blocker inhibits rapidly the activating delayed-rectifier potassium current (IKr), L-type calcium current, and inward sodium current (INa).

HBI-3000 is an experimental drug candidate that is currently in phase II of human clinical trials as an antiarrhythmic agent. Clinical investigation will test the safety and efficacy of HBI-3000 as a treatment for both atrial and ventricular arrhythmias.