Related Research Articles
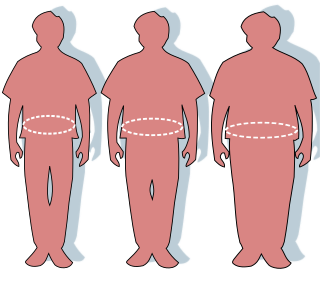
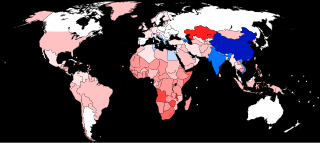
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it can potentially have negative effects on health. People are classified as obese when their body mass index (BMI)—a person's weight divided by the square of the person's height—is over 30 kg/m2; the range 25–30 kg/m2 is defined as overweight. Some East Asian countries use lower values to calculate obesity. Obesity is a major cause of disability and is correlated with various diseases and conditions, particularly cardiovascular diseases, type 2 diabetes, obstructive sleep apnea, certain types of cancer, and osteoarthritis.

Maternal death or maternal mortality is defined in slightly different ways by several different health organizations. The World Health Organization (WHO) defines maternal death as the death of a pregnant mother due to complications related to pregnancy, underlying conditions worsened by the pregnancy or management of these conditions. This can occur either while she is pregnant or within six weeks of resolution of the pregnancy. The CDC definition of pregnancy-related deaths extends the period of consideration to include one year from the resolution of the pregnancy. Pregnancy associated death, as defined by the American College of Obstetricians and Gynecologists (ACOG), are all deaths occurring within one year of a pregnancy resolution. Identification of pregnancy associated deaths is important for deciding whether or not the pregnancy was a direct or indirect contributing cause of the death.

Population ageing is an increasing median age in a population because of declining fertility rates and rising life expectancy. Most countries have rising life expectancy and an ageing population, trends that emerged first in developed countries but are now seen in virtually all developing countries. That is the case for every country in the world except the 18 countries designated as "demographic outliers" by the United Nations. The aged population is currently at its highest level in human history. The UN predicts the rate of population ageing in the 21st century will exceed that of the previous century. The number of people aged 60 years and over has tripled since 1950 and reached 600 million in 2000 and surpassed 700 million in 2006. It is projected that the combined senior and geriatric population will reach 2.1 billion by 2050. Countries vary significantly in terms of the degree and pace of ageing, and the UN expects populations that began ageing later will have less time to adapt to its implications.

Preventive healthcare, or prophylaxis, is the application of healthcare measures to prevent diseases. Disease and disability are affected by environmental factors, genetic predisposition, disease agents, and lifestyle choices, and are dynamic processes that begin before individuals realize they are affected. Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.
Health equity arises from access to the social determinants of health, specifically from wealth, power and prestige. Individuals who have consistently been deprived of these three determinants are significantly disadvantaged from health inequities, and face worse health outcomes than those who are able to access certain resources. It is not equity to simply provide every individual with the same resources; that would be equality. In order to achieve health equity, resources must be allocated based on an individual need-based principle.
Multimorbidity, also known as multiple long-term conditions (MLTC), means living with two or more chronic illnesses. For example, a person could have diabetes, heart disease and depression at the same time. Multimorbidity can have a significant impact on people's health and wellbeing. It also poses a complex challenge to healthcare systems which are traditionally focused on individual diseases. Multiple long-term conditions can affect people of any age, but they are more common in older age, affecting more than half of people over 65 years old.
Maternal health is the health of women during pregnancy, childbirth, and the postpartum period. In most cases, maternal health encompasses the health care dimensions of family planning, preconception, prenatal, and postnatal care in order to ensure a positive and fulfilling experience. In other cases, maternal health can reduce maternal morbidity and mortality. Maternal health revolves around the health and wellness of pregnant women, particularly when they are pregnant, at the time they give birth, and during child-raising. WHO has indicated that even though motherhood has been considered as a fulfilling natural experience that is emotional to the mother, a high percentage of women develop health problems and sometimes even die. Because of this, there is a need to invest in the health of women. The investment can be achieved in different ways, among the main ones being subsidizing the healthcare cost, education on maternal health, encouraging effective family planning, and ensuring progressive check up on the health of women with children. Maternal morbidity and mortality particularly affects women of color and women living in low and lower-middle income countries.

In medicine, rural health or rural medicine is the interdisciplinary study of health and health care delivery in rural environments. The concept of rural health incorporates many fields, including wilderness medicine, geography, midwifery, nursing, sociology, economics, and telehealth or telemedicine.
Eileen M. Crimmins is the AARP Chair in Gerontology at the USC Davis School of Gerontology of the University of Southern California. Her work focuses on the connections between socioeconomic factors and life expectancy and other health outcomes.

Frailty is a common geriatric syndrome that embodies an elevated risk of catastrophic declines in health and function among older adults. Frailty is a condition associated with ageing, and it has been recognized for centuries. It is a marker of a more widespread syndrome of frailty, with associated weakness, slowing, decreased energy, lower activity, and, when severe, unintended weight loss. As a frequent clinical syndrome in the elderly, various health risks are linked to health deterioration and frailty in older age, such as falls, disability, hospitalization, and mortality. Generally, frailty refers to older adults who lose independence. It also links to the experiences of losing dignity due to social and emotional isolation risk. Frailty has been identified as a risk factor for the development of dementia.
The human sex ratio is the ratio of males to females in a population in the context of anthropology and demography. In humans, the natural sex ratio at birth is slightly biased towards the male sex. It is estimated to be about 1.05 or 1.06 or within a narrow range from 1.03 to 1.06 males per female.
Cognitive epidemiology is a field of research that examines the associations between intelligence test scores and health, more specifically morbidity and mortality. Typically, test scores are obtained at an early age, and compared to later morbidity and mortality. In addition to exploring and establishing these associations, cognitive epidemiology seeks to understand causal relationships between intelligence and health outcomes. Researchers in the field argue that intelligence measured at an early age is an important predictor of later health and mortality differences.
Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance. The United States spends more on healthcare than any other country, both in absolute terms and as a percentage of GDP; however, this expenditure does not necessarily translate into better overall health outcomes compared to other developed nations. Coverage varies widely across the population, with certain groups, such as the elderly and low-income individuals, receiving more comprehensive care through government programs such as Medicaid and Medicare.
James X. Zhang is an American health economist and health services researcher at the University of Chicago known for his innovative approaches in exploring complex data to measure a range of factors influencing healthcare delivery and outcomes.

Maternal healthcare in Texas refers to the provision of family planning services, abortion options, pregnancy-related services, and physical and mental well-being care for women during the prenatal and postpartum periods. The provision of maternal health services in each state can prevent and reduce the incidence of maternal morbidity and mortality and fetal death.
The weathering hypothesis was proposed to account for early health deterioration as a result of cumulative exposure to experiences of social, economic, and political adversity. It is well documented that minority groups and marginalized communities suffer from poorer health outcomes. This may be due to a multitude of stressors including prejudice, social alienation, institutional bias, political oppression, economic exclusion, and racial discrimination. The weathering hypothesis proposes that the cumulative burden of these stressors as individuals age is "weathering", and the increased weathering experienced by minority groups compared to others can account for differences in health outcomes. In recent years, the biological plausibility of the weathering hypothesis has been investigated in studies evaluating the physiological effects of social, environmental and political stressors among marginalized communities. This has led to more widespread use of the weathering hypothesis as a framework for explaining health disparities on the basis of differential exposure to racially based stressors. Researchers have also identified patterns connecting weathering to biological phenomena associated with stress and aging, such as allostatic load, epigenetics, telomere shortening, and accelerated brain aging.
The male-female health-survival paradox, also known as the morbidity-mortality paradox or gender paradox, is the phenomenon in which female humans experience more medical conditions and disability during their lives, but they unexpectedly live longer than males. This paradox, where females experience greater morbidity (diseases) but lower mortality (death) in comparison to males, is unusual since it is expected that experiencing disease increases the likelihood of death. However, in this case, the part of the population that experiences more disease and disability is the one that lives longer.
Vaping-associated pulmonary injury (VAPI), also known as vaping-associated lung injury (VALI) or e-cigarette, or vaping, product use associated lung injury (E/VALI), is an umbrella term, used to describe lung diseases associated with the use of vaping products that can be severe and life-threatening. Symptoms can initially mimic common pulmonary diagnoses, such as pneumonia, but sufferers typically do not respond to antibiotic therapy. Differential diagnoses have overlapping features with VAPI, including COVID-19. According to a systematic review article, "Initial case reports of vaping-related lung injury date back to 2012, but the ongoing outbreak of EVALI began in the summer of 2019." According to an article in the Radiological Society of North America news published in March 2022, EVALI cases continue to be diagnosed. “EVALI has by no means disappeared,” Dr. Kligerman said. “We continue to see numerous cases, even during the pandemic, many of which are initially misdiagnosed as COVID-19.”
Black maternal mortality in the United States refers to the death of women, specifically those who identify as Black or African American, during or after child delivery. In general, maternal death can be due to a myriad of factors, such as the nature of the pregnancy or the delivery itself, but is not associated with unintentional or secondary causes. In the United States, around 700 women die from pregnancy-related illnesses or complications per year. This number does not include the approximately 50,000 women who experience life-threatening complications during childbirth, resulting in lifelong disabilities and complications. However, there are stark differences in maternal mortality rates for Black American women versus Indigenous American, Alaska Native, and White American women.
Cheryl Cohen is a South African public health researcher who is a professor at the University of the Witwatersrand. She looks to develop evidence-based policy to reduce the burdens of respiratory diseases. During the COVID-19 pandemic. Cohen investigated the rates of COVID-19 in South Africa.
References
- ↑ Fries, James F. (1980). "Aging, Natural Death, and the Compression of Morbidity" (PDF). New England Journal of Medicine. 303 (3): 130–5. doi:10.1056/NEJM198007173030304. PMC 2567746 . PMID 7383070. Archived from the original (PDF) on 2011-08-11. Retrieved 2011-03-31.
- ↑ Vita, Anthony J.; Terry, Richard B.; Hubert, Helen B.; Fries, James F. (1998). "Aging, Health Risks, and Cumulative Disability". New England Journal of Medicine. 338 (15): 1035–41. doi: 10.1056/NEJM199804093381506 . PMID 9535669.
- 1 2 Swartz, Aimee (2008). "James Fries: Healthy Aging Pioneer". American Journal of Public Health. 98 (7): 1163–6. doi:10.2105/AJPH.2008.135731. PMC 2424092 . PMID 18511711.
- ↑ "The compression of morbidity was prophetic in the sense that Jim looked at the reduction of morbidity and disability at a time when most gerontologists and epidemiologists thought we would see a pandemic of disability." —Richard Suzman, quoted in Swartz 2008
- ↑ Mor, Vincent (2005). "The Compression of Morbidity Hypothesis: A Review of Research and Prospects for the Future". Journal of the American Geriatrics Society. 53 (9s): S308–S309. doi:10.1111/j.1532-5415.2005.53496.x. PMID 16131359. S2CID 24003528.
- ↑ Crimmins, Eileen M.; Beltrán-Sánchez, Hiram (2011-01-01). "Mortality and Morbidity Trends: Is There Compression of Morbidity?". The Journals of Gerontology: Series B. 66B (1): 75–86. doi:10.1093/geronb/gbq088. ISSN 1079-5014. PMC 3001754 . PMID 21135070.
- ↑ "APA PsycNet".