A head injury is any injury that results in trauma to the skull or brain. The terms traumatic brain injury and head injury are often used interchangeably in the medical literature. Because head injuries cover such a broad scope of injuries, there are many causes—including accidents, falls, physical assault, or traffic accidents—that can cause head injuries.

Neurotrauma, brain damage or brain injury (BI) is the destruction or degeneration of brain cells. Brain injuries occur due to a wide range of internal and external factors. In general, brain damage refers to significant, undiscriminating trauma-induced damage.

Shaken baby syndrome (SBS), also known as abusive head trauma (AHT), is a medical condition in children younger than five years old, generally caused by blunt trauma, vigorous shaking, or a combination of both. SBS is the leading cause of fatal head injuries in children under two, with a risk of death of about 25%. The most common symptoms include retinal bleeds, multiple fractures of the long bones, and subdural hematomas.

A concussion, also known as a mild traumatic brain injury (mTBI), is a head injury that temporarily affects brain functioning. Symptoms may include loss of consciousness; memory loss; headaches; difficulty with thinking, concentration, or balance; nausea; blurred vision; dizziness; sleep disturbances, and mood changes. Any of these symptoms may begin immediately, or appear days after the injury. Concussion should be suspected if a person indirectly or directly hits their head and experiences any of the symptoms of concussion. Symptoms of a concussion may be delayed by 1–2 days after the accident. It is not unusual for symptoms to last 2 weeks in adults and 4 weeks in children. Fewer than 10% of sports-related concussions among children are associated with loss of consciousness.

A subdural hematoma (SDH) is a type of bleeding in which a collection of blood—usually but not always associated with a traumatic brain injury—gathers between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It usually results from tears in bridging veins that cross the subdural space.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

Epidural hematoma is when bleeding occurs between the tough outer membrane covering the brain and the skull. When this condition occurs in the spinal canal, it is known as a spinal epidural hematoma.

A traumatic brain injury (TBI), also known as an intracranial injury, is an injury to the brain caused by an external force. TBI can be classified based on severity ranging from mild traumatic brain injury (mTBI/concussion) to severe traumatic brain injury. TBI can also be characterized based on mechanism or other features. Head injury is a broader category that may involve damage to other structures such as the scalp and skull. TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.
Closed-head injury is a type of traumatic brain injury in which the skull and dura mater remain intact. Closed-head injuries are the leading cause of death in children under 4 years old and the most common cause of physical disability and cognitive impairment in young people. Overall, closed-head injuries and other forms of mild traumatic brain injury account for about 75% of the estimated 1.7 million brain injuries that occur annually in the United States. Brain injuries such as closed-head injuries may result in lifelong physical, cognitive, or psychological impairment and, thus, are of utmost concern with regards to public health.
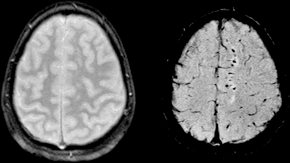
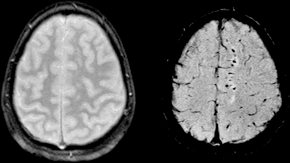
Diffuse axonal injury (DAI) is a brain injury in which scattered lesions occur over a widespread area in white matter tracts as well as grey matter. DAI is one of the most common and devastating types of traumatic brain injury and is a major cause of unconsciousness and persistent vegetative state after severe head trauma. It occurs in about half of all cases of severe head trauma and may be the primary damage that occurs in concussion. The outcome is frequently coma, with over 90% of patients with severe DAI never regaining consciousness. Those who awaken from the coma often remain significantly impaired.

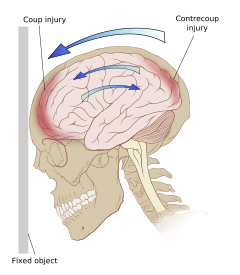
Cerebral contusion, Latin: contusio cerebri, a form of traumatic brain injury, is a bruise of the brain tissue. Like bruises in other tissues, cerebral contusion can be associated with multiple microhemorrhages, small blood vessel leaks into brain tissue. Contusion occurs in 20–30% of severe head injuries. A cerebral laceration is a similar injury except that, according to their respective definitions, the pia-arachnoid membranes are torn over the site of injury in laceration and are not torn in contusion. The injury can cause a decline in mental function in the long term and in the emergency setting may result in brain herniation, a life-threatening condition in which parts of the brain are squeezed past parts of the skull. Thus treatment aims to prevent dangerous rises in intracranial pressure, the pressure within the skull.
Post-concussion syndrome (PCS), also known as persisting symptoms after concussion, is a set of symptoms that may continue for weeks, months, or years after a concussion. PCS is medically classified as a mild traumatic brain injury (TBI). About 35% of people with concussion experience persistent or prolonged symptoms 3 to 6 months after injury. Prolonged concussion is defined as having concussion symptoms for over four weeks following the first accident in youth and for weeks or months in adults.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound. Blunt trauma occurs due to direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, assaults, sports-related injuries, and are notably common among the elderly who experience falls.

Chronic traumatic encephalopathy (CTE) is a neurodegenerative disease linked to repeated trauma to the head. The encephalopathy symptoms can include behavioral problems, mood problems, and problems with thinking. The disease often gets worse over time and can result in dementia.
Second-impact syndrome (SIS) occurs when the brain swells rapidly, and catastrophically, after a person has a second concussion before symptoms from an earlier one have subsided. This second blow may occur minutes, days, or weeks after an initial concussion, and even the mildest grade of concussion can lead to second impact syndrome. The condition is often fatal, and almost everyone who is not killed is severely disabled. The cause of SIS is uncertain, but it is thought that the brain's arterioles lose their ability to regulate their diameter, and therefore lose control over cerebral blood flow, causing massive cerebral edema.
A cerebral laceration is a type of traumatic brain injury that occurs when the tissue of the brain is mechanically cut or torn. The injury is similar to a cerebral contusion; however, according to their respective definitions, the pia-arachnoid membranes are torn over the site of injury in laceration and are not torn in contusion. Lacerations require greater physical force to cause than contusions, but the two types of injury are grouped together in the ICD-9 and ICD-10 classification systems.

Focal and diffuse brain injury are ways to classify brain injury: focal injury occurs in a specific location, while diffuse injury occurs over a more widespread area. It is common for both focal and diffuse damage to occur as a result of the same event; many traumatic brain injuries have aspects of both focal and diffuse injury. Focal injuries are commonly associated with an injury in which the head strikes or is struck by an object; diffuse injuries are more often found in acceleration/deceleration injuries, in which the head does not necessarily contact anything, but brain tissue is damaged because tissue types with varying densities accelerate at different rates. In addition to physical trauma, other types of brain injury, such as stroke, can also produce focal and diffuse injuries. There may be primary and secondary brain injury processes.
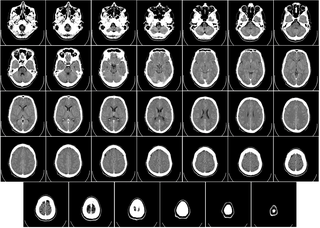
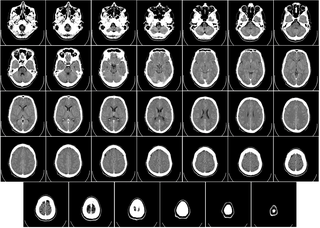
Computed tomography of the head uses a series of X-rays in a CT scan of the head taken from many different directions; the resulting data is transformed into a series of cross sections of the brain using a computer program. CT images of the head are used to investigate and diagnose brain injuries and other neurological conditions, as well as other conditions involving the skull or sinuses; it used to guide some brain surgery procedures as well. CT scans expose the person getting them to ionizing radiation which has a risk of eventually causing cancer; some people have allergic reactions to contrast agents that are used in some CT procedures.
A sports-related traumatic brain injury is a serious accident which may lead to significant morbidity or mortality. Traumatic brain injury (TBI) in sports are usually a result of physical contact with another person or stationary object, These sports may include boxing, gridiron football, field/ice hockey, lacrosse, martial arts, rugby, soccer, wrestling, auto racing, cycling, equestrian, rollerblading, skateboarding, skiing or snowboarding.
A pediatric concussion, also known as pediatric mild traumatic brain injury (mTBI), is a head trauma that impacts the brain capacity. Concussion can affect functional, emotional, cognitive and physical factors and can occur in people of all ages. Symptoms following after the concussion vary and may include confusion, disorientation, lightheadedness, nausea, vomiting, blurred vision, loss of consciousness (LOC) and environment sensitivity. Concussion symptoms may vary based on the type, severity and location of the head injury. Concussion symptoms in infants, children, and adolescents often appear immediately after the injury, however, some symptoms may arise multiple days following the injury leading to a concussion. The majority of pediatric patients recover from the symptoms within one month following the injury. 10-30% of children and adolescents have a higher risk of a delayed recovery or of experiencing concussion symptoms that are persisting.