Related Research Articles

The Diagnostic and Statistical Manual of Mental Disorders is a publication by the American Psychiatric Association (APA) for the classification of mental disorders using a common language and standard criteria. It is the main book for the diagnosis and treatment of mental disorders in the United States and Australia, while in other countries it may be used in conjunction with other documents. The DSM-5 is considered one of the principal guides of psychiatry, along with the International Classification of Diseases (ICD), Chinese Classification of Mental Disorders (CCMD), and the Psychodynamic Diagnostic Manual. However, not all providers rely on the DSM-5 as a guide, since the ICD's mental disorder diagnoses are used around the world and scientific studies often measure changes in symptom scale scores rather than changes in DSM-5 criteria to determine the real-world effects of mental health interventions.
Factitious disorder imposed on self, also known as Munchausen syndrome, is a factitious disorder in which those affected feign or induce disease, illness, injury, abuse, or psychological trauma to draw attention, sympathy, or reassurance to themselves. Munchausen syndrome fits within the subclass of factitious disorder with predominantly physical signs and symptoms, but patients also have a history of recurrent hospitalization, travelling, and dramatic, extremely improbable tales of their past experiences. The term Munchausen syndrome derives its name from the fictional character Baron Munchausen.

Agoraphobia is a mental and behavioral disorder, specifically an anxiety disorder characterized by symptoms of anxiety in situations where the person perceives their environment to be unsafe with no easy way to escape. These situations can include public transit, shopping centers, crowds and queues, or simply being outside their home on their own. Being in these situations may result in a panic attack. Those affected will go to great lengths to avoid these situations. In severe cases, people may become completely unable to leave their homes.

Hypochondriasis or hypochondria is a condition in which a person is excessively and unduly worried about having a serious illness. Hypochondria is an old concept whose meaning has repeatedly changed over its lifespan. It has been claimed that this debilitating condition results from an inaccurate perception of the condition of body or mind despite the absence of an actual medical diagnosis. An individual with hypochondriasis is known as a hypochondriac. Hypochondriacs become unduly alarmed about any physical or psychological symptoms they detect, no matter how minor the symptom may be, and are convinced that they have, or are about to be diagnosed with, a serious illness.

Benign fasciculation syndrome (BFS) is characterized by fasciculation (twitching) of voluntary muscles in the body. The twitching can occur in any voluntary muscle group but is most common in the eyelids, arms, hands, fingers, legs, and feet. The tongue can also be affected. The twitching may be occasional to continuous. BFS must be distinguished from other conditions that include muscle twitches.

Hysteria is a term used to mean ungovernable emotional excess and can refer to a temporary state of mind or emotion. In the nineteenth century, female hysteria was considered a diagnosable physical illness in women. It is assumed that the basis for diagnosis operated under the belief that women are predisposed to mental and behavioral conditions; an interpretation of sex-related differences in stress responses. In the twentieth century, it shifted to being considered a mental illness. Many influential people such as Sigmund Freud and Jean-Martin Charcot dedicated research to hysteria patients.

Claustrophobia is a fear of confined spaces. It is triggered by many situations or stimuli, including elevators, especially when crowded to capacity, windowless rooms, and hotel rooms with closed doors and sealed windows. Even bedrooms with a lock on the outside, small cars, and tight-necked clothing can induce a response in those with claustrophobia. It is typically classified as an anxiety disorder, which often results in panic attacks. The onset of claustrophobia has been attributed to many factors, including a reduction in the size of the amygdala, classical conditioning, or a genetic predisposition to fear small spaces.
Generalized anxiety disorder (GAD) is a mental and behavioral disorder, specifically an anxiety disorder characterized by excessive, uncontrollable and often irrational worry about events or activities. Worry often interferes with daily functioning, and individuals with GAD are often overly concerned about everyday matters such as health, finances, death, family, relationship concerns, or work difficulties. Symptoms may include excessive worry, restlessness, trouble sleeping, exhaustion, irritability, sweating, and trembling.
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usual, causing marked distress, preoccupation with the stressor and its consequences, and functional impairment.
The medical history, case history, or anamnesis of a patient is a set of information the physicians collect over medical interviews. It involves the patient, and eventually people close to them, so to collect reliable/objective information for managing the medical diagnosis and proposing efficient medical treatments. The medically relevant complaints reported by the patient or others familiar with the patient are referred to as symptoms, in contrast with clinical signs, which are ascertained by direct examination on the part of medical personnel. Most health encounters will result in some form of history being taken. Medical histories vary in their depth and focus. For example, an ambulance paramedic would typically limit their history to important details, such as name, history of presenting complaint, allergies, etc. In contrast, a psychiatric history is frequently lengthy and in depth, as many details about the patient's life are relevant to formulating a management plan for a psychiatric illness.
A major depressive episode (MDE) is a period characterized by symptoms of major depressive disorder. Those affected primarily exhibit a depressive mood for at least two weeks or more, and a loss of interest or pleasure in everyday activities. Other symptoms can include feelings of emptiness, hopelessness, anxiety, worthlessness, guilt, irritability, changes in appetite, difficulties in concentration, difficulties remembering details, making decisions, and thoughts of suicide. Insomnia or hypersomnia and aches, pains, or digestive problems that are resistant to treatment may also be present.
Self-diagnosis is the process of diagnosing, or identifying, medical conditions in oneself. It may be assisted by medical dictionaries, books, resources on the Internet, past personal experiences, or recognizing symptoms or medical signs of a condition that a family member previously had or currently has.
Nosophobia, also known as disease phobia or illness anxiety disorder, is the irrational fear of contracting a disease, a type of specific phobia. Primary fears of this kind are fear of contracting HIV infection, pulmonary tuberculosis (phthisiophobia), sexually transmitted infections, cancer (carcinophobia), heart diseases (cardiophobia), and catching the common cold or flu.
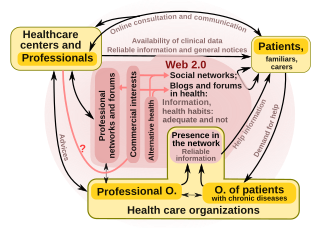
"Health 2.0" is a term introduced in the mid-2000s, as the subset of health care technologies mirroring the wider Web 2.0 movement. It has been defined variously as including social media, user-generated content, and cloud-based and mobile technologies. Some Health 2.0 proponents see these technologies as empowering patients to have greater control over their own health care and diminishing medical paternalism. Critics of the technologies have expressed concerns about possible misinformation and violations of patient privacy.

Medical diagnosis is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as a diagnosis with the medical context being implicit. The information required for a diagnosis is typically collected from a history and physical examination of the person seeking medical care. Often, one or more diagnostic procedures, such as medical tests, are also done during the process. Sometimes the posthumous diagnosis is considered a kind of medical diagnosis.
A depression rating scale is a psychometric instrument (tool), usually a questionnaire whose wording has been validated with experimental evidence, having descriptive words and phrases that indicate the severity of depression for a time period. When used, an observer may make judgements and rate a person at a specified scale level with respect to identified characteristics. Rather than being used to diagnose depression, a depression rating scale may be used to assign a score to a person's behaviour where that score may be used to determine whether that person should be evaluated more thoroughly for a depressive disorder diagnosis. Several rating scales are used for this purpose.
Morgellons is the informal name of a self-diagnosed, scientifically unsubstantiated skin condition in which individuals have sores that they believe contain fibrous material. Morgellons is not well understood, but the general medical consensus is that it is a form of delusional parasitosis, on the psychiatric spectrum. The sores are typically the result of compulsive scratching, and the fibers, when analysed, are consistently found to have originated from cotton and other textiles.
Somatic symptom disorder, also known as somatoform disorder, is defined by one or more chronic physical symptoms that coincide with excessive and maladaptive thoughts, emotions, and behaviors connected to those symptoms. The symptoms are not deliberately produced or feigned, and they may or may not coexist with a known medical ailment.
This article discusses notable unsolved problems in medicine. Many of the problems relate to how drugs work, and to diseases with an unknown cause, the so-called idiopathic diseases.
The Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) is a semi-structured interview aimed at early diagnosis of affective disorders such as depression, bipolar disorder, and anxiety disorder. There are different versions of the test that have use different versions of diagnostic criteria, cover somewhat different diagnoses and use different rating scales for the items. All versions are structured to include interviews with both the child and the parents or guardians, and all use a combination of screening questions and more comprehensive modules to balance interview length and thoroughness.
References
- ↑ Ryen White; Eric Horvitz (2009). "Cyberchondria: Studies of the escalation of medical concerns in Web search". ACM Transactions on Information Systems. 27 (4): 1–37. doi:10.1145/1629096.1629101. S2CID 10984735.
- 1 2 White, R. W.; Horvitz, E (2009). Experiences with web search on medical concerns and self diagnosis (PDF). AMIA Annual Symposium Proceedings. Vol. 2009. pp. 696–700. PMC 2815378 . PMID 20351943.
- ↑ Ferguson, Leila (2013-12-04). "Web research could give you a bad dose of cyberchondria". The Conversation. Retrieved 2017-07-20.
- ↑ Thomas, Elizabeth (11 June 2018). "Be wary of Dr Google". The Asian Age.
- ↑ Oxford English Dictionary #rd Ed. (2003)
- ↑ "The Future Use of the Internet in 4 Countries in Relation to Prescriptions, Physician Communication and Health Information" (PDF). Harris Interactive. 2002-06-20. Retrieved 2006-12-11.
- 1 2 Stone, J; Sharpe, M (2003). "Internet resources for psychiatry and neuropsychiatry". Journal of Neurology, Neurosurgery, and Psychiatry. 74 (1): 10–2. doi:10.1136/jnnp.74.1.10. PMC 1738194 . PMID 12486258.
- ↑ P. Vallely (April 18, 2001). "Are You a Cyberchondriac?". Independent. Archived from the original on July 14, 2001.
- 1 2 "'Cyberchondria' hits web users". BBC News. 2001-04-13. Retrieved 2006-12-11.
- ↑ Showalter, Elaine (1997). Hystories: hysterical epidemics and modern media . New York: Columbia University Press. ISBN 978-0-231-10459-3.
- 1 2 3 White, Ryen W.; Horvitz, Eric (2008). "Cyberchondria: Studies of the Escalation of Medical Concerns in Web Search" (Technical Report (MSR-TR-2008-178)). Microsoft Research . Retrieved 2008-11-26.[ permanent dead link ]
- ↑ Barsky, A. J.; Klerman, G. L. (1983). "Overview: Hypochondriasis, bodily complaints, and somatic styles". American Journal of Psychiatry. 140 (3): 273–283. doi:10.1176/ajp.140.3.273. PMID 6338747.
- ↑ "Microsoft Examines Causes of 'Cyberchondria'". The New York Times. 2008.
- ↑ Amos Tversky; Daniel Kahneman (1974). "Judgment under uncertainty: Heuristics and biases" (PDF). Science . 185 (4157): 1124–1131. Bibcode:1974Sci...185.1124T. doi:10.1126/science.185.4157.1124. JSTOR 1738360. PMID 17835457. S2CID 6196452. Archived from the original (PDF) on 2019-05-28. Retrieved 2008-11-26.
- ↑ White, Ryen W.; Horvitz, Eric (2010). "Predicting escalations of medical queries based on web page structure and content" (PDF). Proc ACM SIGIR Conference on Research and Development in Information Retrieval (SIGIR 2010). p. 769. doi:10.1145/1835449.1835607. ISBN 978-1-4503-0153-4. Archived from the original (PDF) on 2012-10-05.
- 1 2 Donnelly, Laura (2017-09-07). "'Cyberchondria' fuelling anxiety epidemic clogging up hospital clinics". The Telegraph. ISSN 0307-1235 . Retrieved 2018-10-09.
- ↑ "The age of cyberchondria" (PDF). Royal College of Surgeons in Ireland Student Medical Journal. May 2012. Retrieved 9 October 2018.
- ↑ Natasha Wallace (September 7, 2002). "Doctor in the Mouse". Sydney Herald.
- ↑ Davis, Nicola (2018-10-08). "Cyberchondria and cyberhoarding: is internet fuelling new conditions?". The Guardian. Retrieved 2018-10-09.