Related Research Articles

Hippocrates of Kos, also known as Hippocrates II, was a Greek physician of the classical period who is considered one of the most outstanding figures in the history of medicine. He is traditionally referred to as the "Father of Medicine" in recognition of his lasting contributions to the field, such as the use of prognosis and clinical observation, the systematic categorization of diseases, or the formulation of humoural theory. The Hippocratic school of medicine revolutionized ancient Greek medicine, establishing it as a discipline distinct from other fields with which it had traditionally been associated, thus establishing medicine as a profession.
The Nuremberg Code is a set of ethical research principles for human experimentation created by the court in U.S. v Brandt, one of the Subsequent Nuremberg trials that were held after the Second World War.

A physician, medical practitioner, medical doctor, or simply doctor, is a health professional who practices medicine, which is concerned with promoting, maintaining or restoring health through the study, diagnosis, prognosis and treatment of disease, injury, and other physical and mental impairments. Physicians may focus their practice on certain disease categories, types of patients, and methods of treatment—known as specialities—or they may assume responsibility for the provision of continuing and comprehensive medical care to individuals, families, and communities—known as general practice. Medical practice properly requires both a detailed knowledge of the academic disciplines, such as anatomy and physiology, underlying diseases and their treatment—the science of medicine—and also a decent competence in its applied practice—the art or craft of medicine.

The Hippocratic Oath is an oath of ethics historically taken by physicians. It is one of the most widely known of Greek medical texts. In its original form, it requires a new physician to swear, by a number of healing gods, to uphold specific ethical standards. The oath is the earliest expression of medical ethics in the Western world, establishing several principles of medical ethics which remain of paramount significance today. These include the principles of medical confidentiality and non-maleficence. As the seminal articulation of certain principles that continue to guide and inform medical practice, the ancient text is of more than historic and symbolic value. It is enshrined in the legal statutes of various jurisdictions, such that violations of the oath may carry criminal or other liability beyond the oath's symbolic nature.

Informed consent is a principle in medical ethics and medical law that a patient should have sufficient information before making their own free decisions about their medical care. A healthcare provider is often held to have a responsibility to ensure that the consent that a patient gives is informed, and informed consent can apply to a health care intervention on a person, conducting some form of research on a person, or for disclosing a person's information. Informed consent is, in fact, a fundamental principle in the field of health protection, obviously wanting to mark the very close and unavoidable connection between the need for consent and the inviolability of the right to health. A health care provider may ask a patient to consent to receive therapy before providing it, a clinical researcher may ask a research participant before enrolling that person into a clinical trial, and a researcher may ask a research participant before starting some form of controlled experiment. Informed consent is collected according to guidelines from the fields of medical ethics and research ethics.

Assisted suicide is suicide undertaken with the aid of another person. The term usually refers to physician-assisted suicide (PAS), which is suicide that is assisted by a physician or other healthcare provider. Once it is determined that the person's situation qualifies under the physician-assisted suicide laws for that place, the physician's assistance is usually limited to writing a prescription for a lethal dose of drugs.
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families to create a treatment plan and work towards the same common goal. It is important to note that these four values are not ranked in order of importance or relevance and that they all encompass values pertaining to medical ethics. However, a conflict may arise leading to the need for hierarchy in an ethical system, such that some moral elements overrule others with the purpose of applying the best moral judgement to a difficult medical situation. Medical ethics is particularly relevant in decisions regarding involuntary treatment and involuntary commitment.

The Hippocratic Corpus, or Hippocratic Collection, is a collection of around 60 early Ancient Greek medical works strongly associated with the physician Hippocrates and his teachings. The Hippocratic Corpus covers many diverse aspects of medicine, from Hippocrates' medical theories to what he devised to be ethical means of medical practice, to addressing various illnesses. Even though it is considered as a singular corpus that represents Hippocratic medicine, they vary in content, age, style, methods, and views practiced; therefore, authorship is largely unknown. Hippocrates began Western society's development of medicine, through a delicate blending of the art of healing and scientific observations. What Hippocrates was sharing from within his collection of works was not only how to identify symptoms of disease and proper diagnostic practices, but more essentially, he was alluding to his own form of art, "The art of true living and the art of fine medicine combined." The Hippocratic Corpus became the foundation upon which Western medical practice was built.
Medical torture describes the involvement of, or sometimes instigation by, medical personnel in acts of torture, either to judge what victims can endure, to apply treatments which will enhance torture, or as torturers in their own right. Medical torture overlaps with medical interrogation if it involves the use of professional medical expertise to facilitate interrogation or corporal punishment, in the conduct of torturous human experimentation or in providing professional medical sanction and approval for the torture of prisoners. Medical torture also covers torturous scientific experimentation upon unwilling human subjects.

The World Medical Association (WMA) is an international and independent confederation of free professional medical associations representing physicians worldwide. WMA was formally established on September 18, 1947 and has grown to 115 national medical associations, as of 2021, with 1467 Associate Members, including Junior Doctors and medical students. and more than 10 million physicians. WMA is in official relations with the World Health Organization (WHO) and seeks close collaboration with the UN Special Rapporteur on the right to physical and mental health.
The Declaration of Helsinki is a set of ethical principles regarding human experimentation developed originally in 1964 for the medical community by the World Medical Association (WMA). It is widely regarded as the cornerstone document on human research ethics.
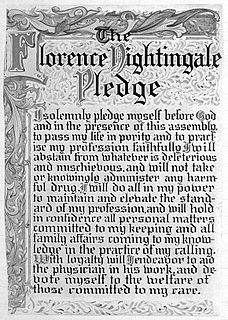
The Nightingale Pledge, named in honour of Florence Nightingale, is a modified version of the Hippocratic Oath. Lystra Gretter and a Committee for the Farrand Training School Grace for Nurses in Detroit, Michigan created the pledge in 1893. Gretter, inspired by the work of Nightingale, the founder of modern nursing, credited the pledge to the work of her committee, but was herself considered "the moving spirit behind the idea" for the pledge.

The International Rehabilitation Council for Torture Victims (IRCT), is an independent, international health professional organization that promotes and supports the rehabilitation of torture victims and works for the prevention of torture worldwide. Based in Denmark, the IRCT is the umbrella organization for over 160 independent torture rehabilitation organizations in 76 countries that treat and assist torture survivors and their families. They advocate for holistic rehabilitation for all victims of torture, which can include access to justice, reparations, and medical, psychological, and psycho-social counseling. The IRCT does this through strengthening the capacity of their membership, enabling an improved policy environment for torture victims, and generating and share knowledge on issues related to the rehabilitation of torture victims. Professionals at the IRCT rehabilitation centers and programs provide treatment for an estimated 100,000 survivors of torture every year. Victims receive multidisciplinary support including medical and psychological care and legal aid. The aim of the rehabilitation process is to empower torture survivors to resume as full a life as possible. In 1988, IRCT, along with founder Inge Genefke, was given the Right Livelihood Award "for helping those whose lives have been shattered by torture to regain their health and personality."
The Declaration of Tokyo is a set of international guidelines for physicians concerning torture and other cruel, inhuman or degrading treatment or punishment in relation to detention and imprisonment, which was adopted in October 1975 during the 29th General assembly of the World Medical Association, and later editorially updated by the WMA in France, May 2005 and 2006. It declares torture to be "contrary to the laws of humanity", and antithetical to the "higher purpose" of the physician, which is to "alleviate the distress of his or her fellow human being." The policy states that doctors should refuse to participate in, condone, or give permission for torture, degradation, or cruel treatment of prisoners or detainees. According to the policy, a prisoner who refuses to eat should not be fed artificially against their will, provided that they are judged to be rational.
The Standing Committee of European Doctors represents national medical associations across Europe.
Medical neutrality refers to a principle of noninterference with medical services in times of armed conflict and civil unrest: physicians must be allowed to care for the sick and wounded, and soldiers must receive care regardless of their political affiliations; all parties must refrain from attacking and misusing medical facilities, transport, and personnel. Concepts comprising the principles of medical neutrality derive from international human rights law, medical ethics and humanitarian law. Medical neutrality may be thought of as a kind of social contract that obligates societies to protect medical personnel in both times of war and peace, and obligates medical personnel to treat all individuals regardless of religion, race, ethnicity, or political affiliation. Violations of medical neutrality constitute crimes outlined in the Geneva Conventions.
The International Code of Medical Ethics was adopted by the General Assembly of the World Medical Association at London in 1949, amended in 1968, 1983 and 2006. It is a code based on the Declaration of Geneva and the main goal is to establish the ethical principles of the physicians worldwide, based on his duties in general, to his patients and to his colleagues.
The Osteopathic Oath is an oath commonly administered to osteopathic physicians who practice osteopathic medicine in the United States. Similar to the Hippocratic Oath, it is a statement of professional values and ethics. The first version of the oath was created in 1938, and the current version of the oath has been in use since 1954. Although taking the oath is not required or legally binding, it is commonly seen as a rite of passage.
World Federation for Medical Education (WFME) is a non-governmental organisation concerned with education and training of medical doctors worldwide. WFME’s main objective is to "enhance the quality of medical education worldwide, with promotion of the highest scientific and ethical standards in medical education". The organisation develops standards for medical education and promotes accreditation of medical schools. It also co-manages the World Directory of Medical Schools.
The CMA Code of Ethics and Professionalism (Code) is a document produced by the Canadian Medical Association. The Code articulates the ethical and professional commitments and responsibilities of the medical profession in Canada.
References
- ↑ "World Medical Association (2017) press release 12 May". Wma.net. 2017-05-08. Retrieved 2018-03-14.
- ↑ "International Code of Medical Ethics". World Medical Association. Archived from the original on 2008-09-20.
- ↑ "The Story of WMA/ who we are/History". Cirp.org. 2002-06-06. Retrieved 2018-03-14.
- ↑ "WMA History". WMA. Archived from the original on 2015-02-06. Retrieved 2013-06-04.
- ↑ "The Oath". Cirp.org. 2002-06-06. Retrieved 2013-06-04.
- ↑ World Medical Association. "WMA Declaration of Geneva". WMA. Retrieved 14 October 2017.
- ↑ Merino, Aruanno, Gelpi, Rancich (2017). "THE PROHIBITION OF EUTHANASIA" AND MEDICAL OATHS OF HIPPOCRATIC STEMMA" (PDF). Acta Bioethica. 23: 171-178 (176). doi:10.4067/S1726-569X2017000100171.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ World Medical Association. "MODERN PHYSICIANS' PLEDGE APPROVED BY WORLD MEDICAL ASSOCIATION". WMA. Retrieved 14 October 2017.
- ↑ WMA , The modern Hippocritic Oath, April 1956
- ↑ World Medical Association, The story of WMA
- ↑ "Queenstown doctor Sam Hazledine's petition for change has worldwide impact". Stuff. 2016-11-02. Retrieved 2022-01-26.
- ↑ World Medical Association WMA Geneva Declaration, 06 November, 2017
- ↑ LoebClassical library, 6 october 2015
- ↑ Claude Pavur , 22 September 2015