Azotemia is a medical condition characterized by abnormally high levels of nitrogen-containing compounds in the blood. It is largely related to insufficient or dysfunctional filtering of blood by the kidneys. It can lead to uremia and acute kidney injury if not controlled.

Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in the large arteries. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure.

Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels tight, the area may feel heavy, and affected joints may be hard to move. Other symptoms depend on the underlying cause.
Baroreceptors are sensors located in the carotid sinus and in the aortic arch. They sense the blood pressure and relay the information to the brain, so that a proper blood pressure can be maintained.

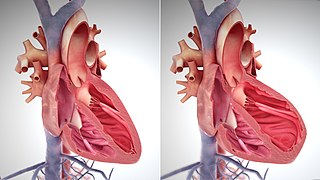
Cardiac output (CO), also known as heart output denoted by the symbols , or , is a term used in cardiac physiology that describes the volume of blood being pumped by the heart, by the left and right ventricle, per unit time. Cardiac output (CO) is the product of the heart rate (HR), i.e. the number of heartbeats per minute (bpm), and the stroke volume (SV), which is the volume of blood pumped from the ventricle per beat; thus, CO = HR × SV. Values for cardiac output are usually denoted as L/min. For a healthy person weighing 70 kg, the cardiac output at rest averages about 5 L/min; assuming a heart rate of 70 beats/min, the stroke volume would be approximately 70 ml.
Diuresis is increased urination and the physiologic process that produces such an increase. It involves extra urine production in the kidneys as part of the body's homeostatic maintenance of fluid balance.

Fluid replacement or fluid resuscitation is the medical practice of replenishing bodily fluid lost through sweating, bleeding, fluid shifts or other pathologic processes. Fluids can be replaced with oral rehydration therapy (drinking), intravenous therapy, rectally such as with a Murphy drip, or by hypodermoclysis, the direct injection of fluid into the subcutaneous tissue. Fluids administered by the oral and hypodermic routes are absorbed more slowly than those given intravenously.

Pulmonary edema(PE), also known as pulmonary congestion, is liquid accumulation in the tissue and air spaces of the lungs. It leads to impaired gas exchange and may cause respiratory failure. It is due to either failure of the left ventricle of the heart to remove blood adequately from the pulmonary circulation, or an injury to the lung tissue or blood vessels of the lung.
Acidosis is a process causing increased acidity in the blood and other body tissues. If not further qualified, it usually refers to acidity of the blood plasma.

Hypovolemia, also known as volume depletion or volume contraction, is a state of abnormally low extracellular fluid in the body. This may be due to either a loss of both salt and water or a decrease in blood volume. Hypovolemia refers to the loss of extracellular fluid and should not be confused with dehydration.

Thirst is the craving for potable fluids, resulting in the basic instinct of animals to drink. It is an essential mechanism involved in fluid balance. It arises from a lack of fluids or an increase in the concentration of certain osmolites, such as sodium. If the water volume of the body falls below a certain threshold or the osmolite concentration becomes too high, structures in the brain detect changes in blood constituents and signal thirst.
Hypovolemic shock is a form of shock caused by severe hypovolemia. It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.

Loop diuretics are diuretics that act at the ascending limb of the loop of Henle in the kidney. They are primarily used in medicine to treat hypertension and edema often due to congestive heart failure or chronic kidney disease. While thiazide diuretics are more effective in patients with normal kidney function, loop diuretics are more effective in patients with impaired kidney function.
Aerospace physiology is the study of the effects of high altitudes on the body, such as different pressures and levels of oxygen. At different altitudes the body may react in different ways, provoking more cardiac output, and producing more erythrocytes. These changes cause more energy waste in the body, causing muscle fatigue, but this varies depending on the level of the altitude.

Metabolic alkalosis is a metabolic condition in which the pH of tissue is elevated beyond the normal range (7.35–7.45). This is the result of decreased hydrogen ion concentration, leading to increased bicarbonate, or alternatively a direct result of increased bicarbonate concentrations. The condition typically cannot last long if the kidneys are functioning properly.

Osmotherapy is the use of osmotically active substances to reduce the volume of intracranial contents. Osmotherapy serves as the primary medical treatment for cerebral edema. The primary purpose of osmotherapy is to improve elasticity and decrease intracranial volume by removing free water, accumulated as a result of cerebral edema, from brain's extracellular and intracellular space into vascular compartment by creating an osmotic gradient between the blood and brain. Normal serum osmolality ranges from 280-290 mOsm/kg and serum osmolality to cause water removal from brain without much side effects ranges from 300-320 mOsm/kg. Usually, 90 mL of space is created in the intracranial vault by 1.6% reduction in brain water content. Osmotherapy has cerebral dehydrating effects. The main goal of osmotherapy is to decrease intracranial pressure (ICP) by shifting excess fluid from brain. This is accomplished by intravenous administration of osmotic agents which increase serum osmolality in order to shift excess fluid from intracellular or extracellular space of the brain to intravascular compartment. The resulting brain shrinkage effectively reduces intracranial volume and decreases ICP.
The Bainbridge reflex, also called the atrial reflex, is an increase in heart rate due to an increase in central venous pressure. Increased blood volume is detected by stretch receptors located in both sides of atria at the venoatrial junctions.
Hypoosmolar hyponatremia is a condition where hyponatremia associated with a low plasma osmolality. The term "hypotonic hyponatremia" is also sometimes used.
High-output heart failure is a heart condition that occurs when the cardiac output is higher than normal due to increased peripheral demand. There is a circulatory overload which may lead to pulmonary edema secondary to an elevated diastolic pressure in the left ventricle. These individuals usually have a normal systolic function but symptoms are those of heart failure. With time, this overload causes systolic failure. Ultimately cardiac output can be reduced to very low levels.
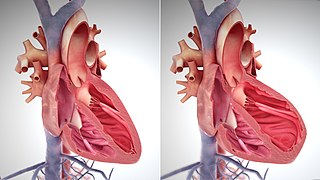
The main pathophysiology of heart failure is a reduction in the efficiency of the heart muscle, through damage or overloading. As such, it can be caused by a wide number of conditions, including myocardial infarction, hypertension and amyloidosis. Over time these increases in workload will produce changes to the heart itself: