Esotropia is a form of strabismus in which one or both eyes turns inward. The condition can be constantly present, or occur intermittently, and can give the affected individual a "cross-eyed" appearance. It is the opposite of exotropia and usually involves more severe axis deviation than esophoria. Esotropia is sometimes erroneously called "lazy eye", which describes the condition of amblyopia; a reduction in vision of one or both eyes that is not the result of any pathology of the eye and cannot be resolved by the use of corrective lenses. Amblyopia can, however, arise as a result of esotropia occurring in childhood: In order to relieve symptoms of diplopia or double vision, the child's brain will ignore or "suppress" the image from the esotropic eye, which when allowed to continue untreated will lead to the development of amblyopia. Treatment options for esotropia include glasses to correct refractive errors, the use of prisms, orthoptic exercises, or eye muscle surgery. The term is from Greek eso meaning "inward" and trope meaning "a turning".
Visual acuity (VA) commonly refers to the clarity of vision, but technically rates an animal's ability to recognize small details with precision. Visual acuity depends on optical and neural factors. Optical factors of the eye influence the sharpness of an image on its retina. Neural factors include the health and functioning of the retina, of the neural pathways to the brain, and of the interpretative faculty of the brain.
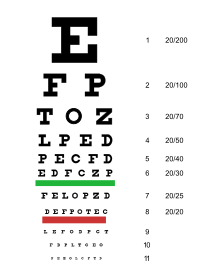
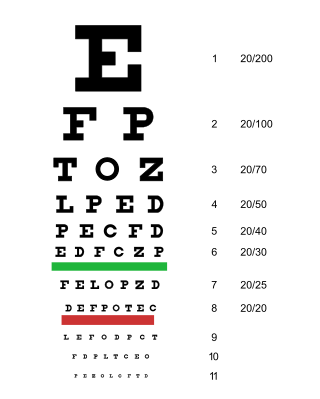
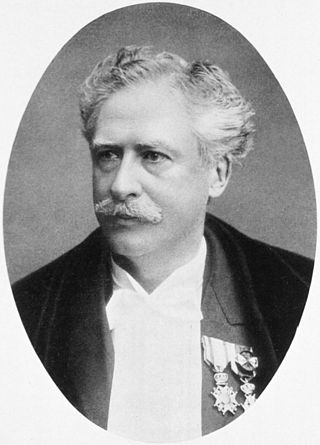
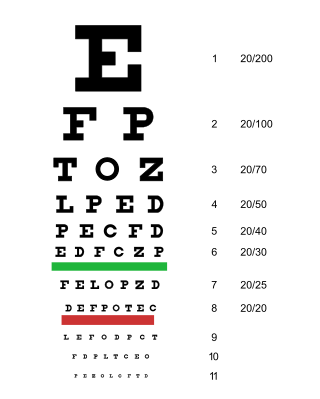
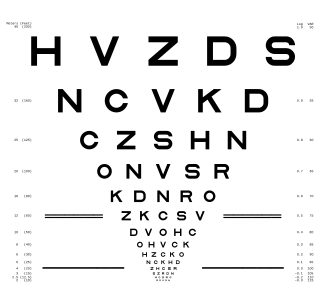
A Snellen chart is an eye chart that can be used to measure visual acuity. Snellen charts are named after the Dutch ophthalmologist Herman Snellen who developed the chart in 1862 as a measurement tool for the acuity formula developed by his professor Franciscus Cornelius Donders. Many ophthalmologists and vision scientists now use an improved chart known as the LogMAR chart.
An eye examination is a series of tests performed to assess vision and ability to focus on and discern objects. It also includes other tests and examinations pertaining to the eyes. Eye examinations are primarily performed by an optometrist, ophthalmologist, or an orthoptist. Health care professionals often recommend that all people should have periodic and thorough eye examinations as part of routine primary care, especially since many eye diseases are asymptomatic.

The Amsler grid, used since 1945, is a grid of horizontal and vertical lines used to monitor a person's central visual field. The grid was developed by Marc Amsler, a Swiss ophthalmologist. It is a diagnostic tool that aids in the detection of visual disturbances caused by changes in the retina, particularly the macula, as well as the optic nerve and the visual pathway to the brain. Amsler grid usually help detecting defects in central 20 degrees of the visual field.
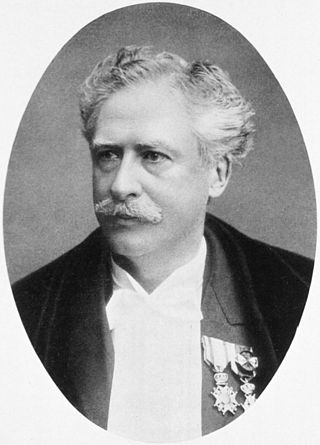
Herman Snellen was a Dutch ophthalmologist who introduced the Snellen chart to study visual acuity (1862). He took over directorship of the Netherlands Hospital for Eye Patients, after Franciscus Donders. He was elected an International Member of the American Philosophical Society in 1894.

The Landolt C, also known as a Landolt ring, Landolt broken ring, or Japanese vision test, is an optotype: a standardized symbol used for testing vision. It was developed by the Swiss-born ophthalmologist Edmund Landolt.

The LEA Vision Test System is a series of pediatric vision tests designed specifically for children who do not know how to read the letters of the alphabet that are typically used in eye charts. There are numerous variants of the LEA test which can be used to assess the visual capabilities of near vision and distance vision, as well as several other aspects of occupational health, such as contrast sensitivity, visual field, color vision, visual adaptation, motion perception, and ocular function and accommodation (eye).

Astigmatism is a type of refractive error due to rotational asymmetry in the eye's refractive power. This results in distorted or blurred vision at any distance. Other symptoms can include eyestrain, headaches, and trouble driving at night. Astigmatism often occurs at birth and can change or develop later in life. If it occurs in early life and is left untreated, it may result in amblyopia.

Eduard Jäger von Jaxtthal was an Austrian ophthalmologist who was a native of Vienna. He was a professor at the University of Vienna, and was son to oculist Friedrich Jäger von Jaxtthal (1784-1871), and grandson to Georg Joseph Beer (1763-1821).

An E chart, also known as a tumbling E chart, is an ophthalmological chart used to measure a patient's visual acuity.

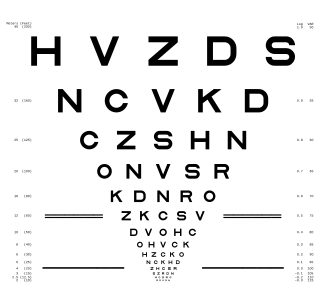
The Golovin–Sivtsev table is a standardized table for testing visual acuity, which was developed in 1923 by Soviet ophthalmologists Sergei Golovin and D. A. Sivtsev. In the USSR, it was the most common table of its kind, and as of 2008 its use is still widespread in several post-Soviet states.

A pinhole occluder is an opaque disk with one or more small holes through it, used by ophthalmologists, orthoptists and optometrists to test visual acuity. The occluder is a simple way to focus light, as in a pinhole camera, temporarily removing the effects of refractive errors such as myopia. Because light passes only through the center of the eye's lens, defects in the shape of the lens have no effect while the occluder is used. In this way, the ophthalmologist, orthoptist or optometrist can estimate the maximum improvement in a patient's vision that can be attained by lenses to correct errors of refraction. This can be used to distinguish visual defects caused by refractive error, which improve when the occluder is used, from other problems, which do not. The pinhole occluder can also be used in testing visual acuity in mydriatic patients. In this case, the pinhole occluder compensates for the inability to contract the iris assisting the eye in obtaining a retinal projection similar to that of a non-cycloplegic eye.
A logMAR chart is a chart consisting of rows of letters that is used by ophthalmologists, orthoptists, optometrists, and vision scientists to estimate visual acuity. The chart was developed at the National Vision Research Institute of Australia in 1976, and is designed to enable a more accurate estimate of acuity than do other charts. For this reason, the LogMAR chart is recommended, particularly in a research setting.

The prism cover test (PCT) is an objective measurement and the gold standard in measuring strabismus, i.e. ocular misalignment, or a deviation of the eye. It is used by ophthalmologists and orthoptists in order to measure the vertical and horizontal deviation and includes both manifest and latent components. Manifest is defined by the eye deviating constantly or intermittently, whereas latent is where the deviation is normally controlled but becomes present when the eyes are dissociated. A PCT reveals the total deviation and cannot distinguish between latent and manifest strabismus as you are using an alternate cover test.

Subjective Refraction is a technique to determine the combination of lenses that will provide the best corrected visual acuity (BCVA). It is a clinical examination used by orthoptists, optometrists and ophthalmologists to determine a patient's need for refractive correction, in the form of glasses or contact lenses. The aim is to improve current unaided vision or vision with current glasses. Glasses must also be comfortable visually. The sharpest final refraction is not always the final script the patient wears comfortably.
Childhood cataract is cataract that occurs at birth or in childhood. It may be congenital or acquired.
The Jaeger chart is an eye chart used in testing near vision acuity. It is a card on which paragraphs of text are printed, with the text sizes increasing from 0.37 mm to 2.5 mm. This card is to be held by a patient at a fixed distance from the eye dependent on the J size being read. The smallest print that the patient can read determines their visual acuity. The original 1867 chart had a text containing seven paragraphs and a corresponding seven-point scale.

Louise Littig Sloan was an American ophthalmologist and vision scientist. She is credited for being a pioneer of the sub-division of clinical vision research, contributing more than 100 scientific articles in which she either authored or co-authored. Her most notable work was in the area of visual acuity testing where she developed and improved equipment. Sloan received her Ph.D. from Bryn Mawr College in experimental psychology. She spent a short period of time in both Bryn Mawr's experimental psychology program as well as the Department of Ophthalmology at Harvard Medical School. The majority of her career, however, was spent at Johns Hopkins Wilmer Eye Institute where she directed the Wilmer Laboratory of Physiological Optics for 44 years. In 1971, Sloan was the second woman awarded the prestigious Edgar D. Tillyer Award by Optica (formerly Optical Society for her many achievements in the field of vision.
The MNREAD acuity chart or Minnesota low vision reading chart is a text based chart used to measure near visual acuity in people with normal or low vision. It can also be used to measure maximum reading speed, critical print size and the reading accessibility index of a person. Digital and printed types of charts are available.