Nephrology is a specialty of adult internal medicine and pediatric medicine that concerns the study of the kidneys, specifically normal kidney function and kidney disease, the preservation of kidney health, and the treatment of kidney disease, from diet and medication to renal replacement therapy. The word “renal” is an adjective meaning “relating to the kidneys”, and its roots are French or late Latin. Whereas according to some opinions, "renal" and "nephro" should be replaced with "kidney" in scientific writings such as "kidney medicine" or "kidney replacement therapy", other experts have advocated preserving the use of renal and nephro as appropriate including in "nephrology" and "renal replacement therapy", respectively.
Forensic pathology is pathology that focuses on determining the cause of death by examining a corpse. A post mortem examination is performed by a medical examiner or forensic pathologist, usually during the investigation of criminal law cases and civil law cases in some jurisdictions. Coroners and medical examiners are also frequently asked to confirm the identity of a corpse.

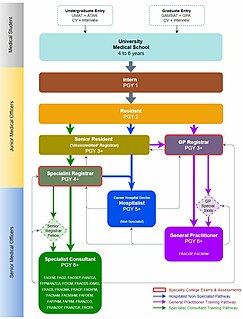
In the medical profession, a general practitioner (GP) is a medical doctor who treats acute and chronic illnesses and provides preventive care and health education to patients of all ages.
Internal medicine or general internal medicine is the medical specialty dealing with the prevention, diagnosis, and treatment of internal diseases. Physicians specializing in internal medicine are called internists, or physicians in Commonwealth nations. Internists are skilled in the management of patients who have undifferentiated or multi-system disease processes. Internists care for hospitalized and ambulatory patients and may play a major role in teaching and research. Internal medicine and family medicine are often confused as equivalent in the Commonwealth nations.
A radiation oncologist is a specialist physician who uses ionizing radiation in the treatment of cancer. Radiation oncology is one of the three primary specialties, the other two being surgical and medical oncology, involved in the treatment of cancer. Radiation can be given as a curative modality, either alone or in combination with surgery and/or chemotherapy. It may also be used palliatively, to relieve symptoms in patients with incurable cancers. A radiation oncologist may also use radiation to treat some benign diseases, including benign tumors. In some countries, radiotherapy and chemotherapy are controlled by a single oncologist who is a "clinical oncologist". Radiation oncologists work closely with other physicians such as surgical oncologists, interventional radiologists, internal medicine subspecialists, and medical oncologists, as well as medical physicists and technicians as part of the multi-disciplinary cancer team. Radiation oncologists undergo four years of oncology-specific training whereas oncologists who deliver chemotherapy have two years of additional training in cancer care during fellowship after internal medicine residency in the United States.

Anesthesiology, or anaesthesiology, is the medical specialty concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialized in anesthesiology is called an anesthesiologist or anesthetist, depending on the country. In some countries, the terms are effectively synonymous, but in other countries they refer to different positions and the term "anesthetist" is only used for non-physicians, such as nurse anesthetists.

Doctor of Medicine is a medical degree, the meaning of which varies between different jurisdictions. In the United States, and some other countries, the M.D. denotes a professional graduate degree. This generally arose because many in 18th-century medical professions trained in Scotland, which used the M.D. degree nomenclature. In England, however, Bachelor of Medicine, Bachelor of Surgery was used and eventually in the 19th century became the standard in Scotland too. Thus, in the United Kingdom, Ireland and other countries, the M.D. is a research doctorate, higher doctorate, honorary doctorate or applied clinical degree restricted to those who already hold a professional degree (Bachelor's/Master's/Doctoral) in medicine; in those countries, the equivalent professional to the North American and some others use of M.D. is still typically titled Bachelor of Medicine, Bachelor of Surgery (M.B.B.S.).
A medical school is a tertiary educational institution, or part of such an institution, that teaches medicine, and awards a professional degree for physicians and surgeons. Such medical degrees include the Bachelor of Medicine, Bachelor of Surgery, Master of Medicine, Doctor of Medicine (M.D.), or Doctor of Osteopathic Medicine (D.O.). Many medical schools offer additional degrees, such as a Doctor of Philosophy (Ph.D.), master's degree (M.Sc.) or other post-secondary education.
Membership of the Royal Colleges of Physicians of the United Kingdom is a postgraduate medical diploma in the United Kingdom (UK). The examinations are run by the Federation of the Medical Royal Colleges – the Royal College of Physicians of London, the Royal College of Physicians of Edinburgh, and the Royal College of Physicians and Surgeons of Glasgow. The three Royal Colleges of Physicians share this common three part assessment in general medicine which consists of two written parts and one clinical examination. Examinations are held throughout the UK and in overseas centres.

Residency or postgraduate training is specifically a stage of graduate medical education. It refers to a qualified physician or podiatrist (DPM) who practices medicine or podiatry, respectively, usually in a hospital or clinic, under the direct or indirect supervision of a senior medical clinician registered in that specialty such as an attending physician or consultant. In many jurisdictions, successful completion of such training is a requirement in order to obtain an unrestricted license to practice medicine, and in particular a license to practice a chosen specialty. An individual engaged in such training may be referred to as a resident, registrar or trainee depending on the jurisdiction. Residency training may be followed by fellowship or sub-specialty training.
The Royal Australian and New Zealand College of Radiologists (RANZCR) is the leading professional organisation for the promotion of the science and practice of the medical specialties of clinical radiology and radiation oncology in Australia and New Zealand. The College has members throughout the world. RANZCR provides the educational curricula for medical graduates training to enter the specialties.
There are a number of professional degrees in dentistry offered by dental schools in various countries around the world.

The Australasian College for Emergency Medicine (ACEM), based in Melbourne Australia, is the primary training body for specialist emergency physicians in Australia and New Zealand. The college is recognised by the Australian Medical Council and Medical Council of New Zealand as such and provides services for approximately 2700 Fellows and 2600 Trainees.
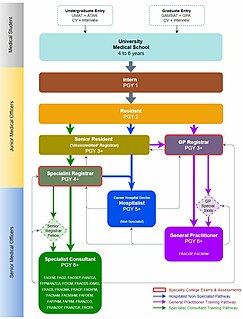
Medical education in Australia includes the educational activities involved in the initial and ongoing training of Medical Practitioners. In Australia, medical education begins in Medical School; upon graduation it is followed by a period of pre-vocational training including Internship and Residency; thereafter, enrolment into a specialist-vocational training program as a Registrar eventually leads to fellowship qualification and recognition as a fully qualified Specialist Medical Practitioner. Medical education in Australia is facilitated by Medical Schools and the Medical Specialty Colleges, and is regulated by the Australian Medical Council (AMC) and Australian Health Practitioners Regulatory Agency (AHPRA) of which includes the Medical Board of Australia where medical practitioners are registered nationally.
The Royal Australasian College of Physicians (RACP) is a not-for-profit professional organisation responsible for training and educating physicians and trainee physicians in Australia and New Zealand.
A phlebologist is a medical specialist in the diagnosis and treatment of disorders of venous origin. The specialty of phlebology has developed to enable physicians sharing an interest in venous disease and health to share knowledge and experience despite being trained in a variety of backgrounds such as dermatology, vascular surgery, haematology, interventional radiology or general medicine. Diagnostic techniques used include the patient's history and physical examination, venous imaging techniques in particular vascular ultrasound and laboratory evaluation related to venous thromboembolism. The American Medical Association and the American Osteopathic Association has added phlebology to their list of self-designated practice specialties.

The Royal Australian and New Zealand College of Psychiatrists (RANZCP) is the principal organisation representing the medical specialty of psychiatry in Australia and New Zealand and has responsibility for training, examining and awarding the qualification of Fellowship of the College (FRANZCP) to medical practitioners.
The College of Intensive Care Medicine (CICM), also known by its longer and more complete name, the College of Intensive Care Medicine of Australia and New Zealand, is the medical specialty college statutorily responsible for the training and accreditation of intensive care medical specialists in Australia and New Zealand.
The Royal Australasian College of Medical Administrators (RACMA) is an accredited specialist medical college comprising medical practitioners with specialist training in management and leadership of health services and systems. Fellows of the college combine clinical knowledge, skill, and judgement and apply this at an organisation wide level. This may include administering or managing a hospital or other health service, or developing health operational policy, or planning or purchasing health services. The college is responsible for the training of medical professionals as specialist health leaders in Australia and New Zealand and has responsibility for assessing candidates and awarding the qualification of Fellowship of the college (FRACMA) to medical practitioners.
The Human Genetics Society of Australasia (HGSA) is a membership organization for individuals in the field of human genetics who primarily practise in the Oceania region. Members typically hold both a qualification in human genetics and work in the field. Membership is drawn from clinical, laboratory and academic specialties. Members include clinical geneticists; genetic counsellors; laboratory scientists ; and academics.