Mortality rate, or death rate, is a measure of the number of deaths in a particular population, scaled to the size of that population, per unit of time. Mortality rate is typically expressed in units of deaths per 1,000 individuals per year; thus, a mortality rate of 9.5 in a population of 1,000 would mean 9.5 deaths per year in that entire population, or 0.95% out of the total. It is distinct from "morbidity", which is either the prevalence or incidence of a disease, and also from the incidence rate.

Child mortality is the mortality of children under the age of five. The child mortality rate, also under-five mortality rate, refers to the probability of dying between birth and exactly five years of age expressed per 1,000 live births.
In terms of available healthcare and health status Sierra Leone is rated very poorly. Globally, infant and maternal mortality rates remain among the highest. The major causes of illness within the country are preventable with modern technology and medical advances. Most deaths within the country are attributed to nutritional deficiencies, lack of access to clean water, pneumonia, diarrheal diseases, anemia, malaria, tuberculosis and HIV/AIDS.
Health in the Comoros continues to face public health problems characteristic of developing countries. After Comoros's independence in 1975, the French withdrew their medical teams, leaving the three islands' already rudimentary health care system in a state of severe crisis. French assistance was eventually resumed, and other nations also contributed medical assistance to the young republic.
Health in Indonesia is affected by a number of factors. Indonesia has over 26,000 health care facilities; 2,000 hospitals, 9,000 community health centres and private clinics, 1,100 dentist clinics and 1,000 opticians. The country lacks doctors with only 0.4 doctors per 1,000 population. In 2018, Indonesia's healthcare spending was US$38.3 billion, 4.18% of their GDP, and is expected to rise to US$51 billion in 2020.
Health care services in Nepal are provided by both public and private sectors and are generally regarded as failing to meet international standards. Prevalence of disease is significantly higher in Nepal than in other South Asian countries, especially in rural areas. Moreover, the country's topographical and sociological diversity results in periodic epidemics of infectious diseases, epizootics and natural hazards such as floods, forest fires, landslides, and earthquakes. But, recent surge in Non communicable diseases has emerged as the main public health concern and this accounts for more than two-thirds of total mortality in country. A large section of the population, particularly those living in rural poverty, are at risk of infection and mortality by communicable diseases, malnutrition and other health-related events. Nevertheless, some improvements in health care can be witnessed; most notably, there has been significant improvement in the field of maternal health. These improvements include:

The Tajikistan health system is influenced by the former Soviet legacy. It is ranked as the poorest country within the WHO European region, including the lowest total health expenditure per capita. Tajikistan is ranked 129th as Human Development Index of 188 countries, with an Index of 0.627 in 2016. In 2016, the SDG Index value was 56. In Tajikistan health indicators such as infant and maternal mortality rates are among the highest of the former Soviet republics. In the post-Soviet era, life expectancy has decreased because of poor nutrition, polluted water supplies, and increased incidence of cholera, malaria, tuberculosis, and typhoid. Because the health care system has deteriorated badly and receives insufficient funding and because sanitation and water supply systems are in declining condition, Tajikistan has a high risk of epidemic disease.
Healthcare in Laos is provided by both the private and public sector. It is limited in comparison with other countries. Western medical care is available in some locations, but remote areas and ethnic groups are underserved. Public spending on healthcare is low compared with neighbouring countries. Still, progress has been made since Laos joined the World Health Organization in 1950: life expectancy at birth rose to 66 years by 2015; malaria deaths and tuberculosis prevalence have plunged; and the maternal mortality ratio (MMR) has declined by 75 percent.

Niger is a landlocked country located in West Africa and has Libya, Chad, Nigeria, Benin, Mali, Burkina Faso, and Algeria as its neighboring countries. Niger was French territory that got its independence in 1960 and its official language is French. Niger has an area of 1.267 million square kilometres, nevertheless, 80% of its land area spreads through the Sahara Desert.

The quality of health in Cambodia is rising along with its growing economy. The public health care system has a high priority from the Cambodian government and with international help and assistance, Cambodia has seen some major and continuous improvements in the health profile of its population since the 1980s, with a steadily rising life expectancy.
The current population of Myanmar is 54.05 million. It was 27.27 million in 1970. The general state of healthcare in Myanmar is poor. The military government of 1962-2011 spent anywhere from 0.5% to 3% of the country's GDP on healthcare. Healthcare in Myanmar is consistently ranked among the lowest in the world. In 2015, in congruence with a new democratic government, a series of healthcare reforms were enacted. In 2017, the reformed government spent 5.2% of GDP on healthcare expenditures. Health indicators have begun to improve as spending continues to increase. Patients continue to pay the majority of healthcare costs out of pocket. Although, out of pocket costs were reduced from 85% to 62% from 2014 to 2015. They continue to drop annually. The global average of healthcare costs paid out of pocket is 32%. Both public and private hospitals are understaffed due to a national shortage of doctors and nurses. Public hospitals lack many of the basic facilities and equipment. WHO consistently ranks Myanmar among the worst nations in healthcare.
Botswana's healthcare system has been steadily improving and expanding its infrastructure to become more accessible. The country's position as an upper middle-income country has allowed them to make strides in universal healthcare access for much of Botswana's population. The majority of the Botswana's 2.3 million inhabitants now live within five kilometers of a healthcare facility. As a result, the infant mortality and maternal mortality rates have been on a steady decline. The country's improving healthcare infrastructure has also been reflected in an increase of the average life expectancy from birth, with nearly all births occurring in healthcare facilities.

A landlocked sub-Saharan country, Burkina Faso is among the poorest countries in the world—44 percent of its population lives below the international poverty line of US$1.90 per day —and it ranks 185th out of 188 countries on UNDP's 2016 Human Development Index .Rapid population growth, gender inequality, and low levels of educational attainment contribute to food insecurity and poverty in Burkina Faso. The total population is just over 20 million with the estimated population growth rate is 3.1 percent per year and seven out of 10 Burkinabe are younger than 30. Total health care expenditures were an estimated 5% of GDP. Total expenditure on health per capita is 82 in 2014.

The Human Rights Measurement Initiative finds that Cameroon is fulfilling 61.0% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Cameroon achieves 81.7% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 70.5% of what is expected based on the nation's level of income. Cameroon falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 30.9% of what the nation is expected to achieve based on the resources (income) it has available.
The Republic of Moldova has a universal health care system.

Lesotho's Human development index value for 2018 was 0.518—which put the country in the low human development category—positioning it at 164 out of 189 countries and territories. Health care services in Lesotho are delivered primarily by the government and the Christian Health Association of Lesotho. Access to health services is difficult for many people, especially in rural areas. The country's health system is challenged by the relentless increase of the burden of disease brought about by AIDS, and a lack of expertise and human resources. Serious emergencies are often referred to neighbouring South Africa. The largest contribution to mortality in Lesotho are communicable diseases, maternal, perinatal and nutritional conditions.
Zambia is a landlocked country in Sub Saharan Africa which experiences a burden of both communicable and non-communicable diseases. In line with WHO agenda for equity in health, it has adopted the Universal Health Coverage agenda to mitigate the challenges faced within the health sector. The Ministry of Health (MOH) provides information pertaining to Zambian health. The main focus of the Ministry of Health has been provision of uninterrupted care with emphasis on health systems strengthening and services via the primary health care approach.
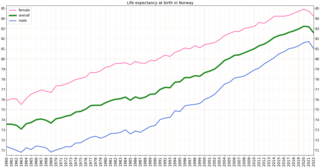
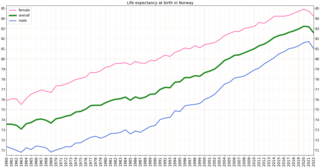
Health in Norway, with its early history of poverty and infectious diseases along with famines and epidemics, was poor for most of the population at least into the 1800s. The country eventually changed from a peasant society to an industrial one and established a public health system in 1860. Due to the high life expectancy at birth, the low under five mortality rate and the fertility rate in Norway, it is fair to say that the overall health status in the country is generally good.

Hospitals and small medical centers and posts are found throughout the island of Madagascar, although they are concentrated in urban areas and particularly in Antananarivo. In addition to the high expense of medical care relative to the average Malagasy income, the prevalence of trained medical professionals remains extremely low.

Life expectancy in Albania was estimated at 77.59 years, in 2014, ranking 51st in the world, and outperforming a number of European Union countries, such as Hungary, Poland and the Czech Republic. In 2016 it was 74 for men and 79 for women. The most common causes of death are circulatory diseases followed by cancerous illnesses. Demographic and Health Surveys completed a survey in April 2009, detailing various health statistics in Albania, including male circumcision, abortion and more.