Related Research Articles
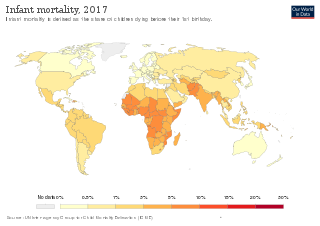
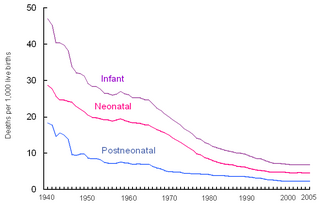
Infant mortality is the death of an infant before the infant's first birthday. The occurrence of infant mortality in a population can be described by the infant mortality rate (IMR), which is the number of deaths of infants under one year of age per 1,000 live births. Similarly, the child mortality rate, also known as the under-five mortality rate, compares the death rate of children up to the age of five.

Mortality rate, or death rate, is a measure of the number of deaths in a particular population, scaled to the size of that population, per unit of time. Mortality rate is typically expressed in units of deaths per 1,000 individuals per year; thus, a mortality rate of 9.5 in a population of 1,000 would mean 9.5 deaths per year in that entire population, or 0.95% out of the total. It is distinct from "morbidity", which is either the prevalence or incidence of a disease, and also from the incidence rate.

Maternal death or maternal mortality is defined in slightly different ways by several different health organizations. The World Health Organization (WHO) defines maternal death as the death of a pregnant mother due to complications related to pregnancy, underlying conditions worsened by the pregnancy or management of these conditions. This can occur either while they are pregnant or within six weeks of resolution of the pregnancy. The CDC definition of pregnancy-related deaths extends the period of consideration to include one year from the resolution of the pregnancy. Pregnancy associated death, as defined by the American College of Obstetricians and Gynecologists (ACOG), are all deaths occurring within one year of a pregnancy resolution. Identification of pregnancy associated deaths is important for deciding whether or not the pregnancy was a direct or indirect contributing cause of the death.
Perinatal mortality (PNM) is the death of a fetus or neonate and is the basis to calculate the perinatal mortality rate. Perinatal means "relating to the period starting a few weeks before birth and including the birth and a few weeks after birth."
Health in Cuba refers to the overall health of the population of Cuba. Like the rest of the Cuban economy, Cuban medical care suffered following the end of Soviet subsidies in 1991; the stepping up of the US embargo against Cuba at this time also had an effect.

Malaysia is classified by The World Bank as upper middle income country and is attempting to achieve high-income status by 2020 and to move further up the value-added production chain by attracting investments in high technology, knowledge-based industries and services. Malaysia's HDI value for 2015 was recorded at 0.789 and HDI rank no 59 out of 188 countries and territories on the United Nations Development Programme's Human Development Index. In 2016, the population of Malaysia is 31 million; Total expenditure on health per capita is 1040; Total expenditure on health as % of GDP (2014) was 4.2 Gross national income (GNI) per capita was recorded at 24,620

The Tajikistan health system is influenced by the former Soviet legacy. It is ranked as the poorest country within the WHO European region, including the lowest total health expenditure per capita. Tajikistan is ranked 129th as Human Development Index of 188 countries, with an Index of 0.627 in 2016. In 2016, the SDG Index value was 56. In Tajikistan health indicators such as infant and maternal mortality rates are among the highest of the former Soviet republics. In the post-Soviet era, life expectancy has decreased because of poor nutrition, polluted water supplies, and increased incidence of cholera, malaria, tuberculosis, and typhoid. Because the health care system has deteriorated badly and receives insufficient funding and because sanitation and water supply systems are in declining condition, Tajikistan has a high risk of epidemic disease.
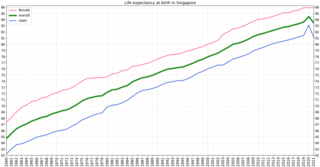
Singapore is one of the wealthiest countries in the world, with a gross domestic product (GDP) per capita of more than $57,000. Life expectancy at birth is 82.3 and infant mortality is 2.7 per 1000 live births. The population is ageing and by 2030, 20% will be over 65. However it is estimated that about 85% of those over 65 are healthy and reasonably active. Singapore has a universal health care system.

Niger is a landlocked country located in West Africa and has Libya, Chad, Nigeria, Benin, Mali, Burkina Faso, and Algeria as its neighboring countries. Niger was French territory that got its independence in 1960 and its official language is French. Niger has an area of 1.267 million square kilometres, nevertheless, 80% of its land area spreads through the Sahara Desert.

Health problems have been a long-standing issue limiting development in the Democratic Republic of the Congo.
The current population of Myanmar is 54.05 million. It was 27.27 million in 1970. The general state of healthcare in Myanmar is poor. The military government of 1962-2011 spent anywhere from 0.5% to 3% of the country's GDP on healthcare. Healthcare in Myanmar is consistently ranked among the lowest in the world. In 2015, in congruence with a new democratic government, a series of healthcare reforms were enacted. In 2017, the reformed government spent 5.2% of GDP on healthcare expenditures. Health indicators have begun to improve as spending continues to increase. Patients continue to pay the majority of healthcare costs out of pocket. Although, out of pocket costs were reduced from 85% to 62% from 2014 to 2015. They continue to drop annually. The global average of healthcare costs paid out of pocket is 32%. Both public and private hospitals are understaffed due to a national shortage of doctors and nurses. Public hospitals lack many of the basic facilities and equipment. WHO consistently ranks Myanmar among the worst nations in healthcare.
According to the World Bank income level classification, Portugal is considered to be a high income country. Its population was of 10,283,822 people, by 1 July 2019. WHO estimates that 21.7% of the population is 65 or more years of age (2018), a proportion that is higher than the estimates for the WHO European Region.

The Human Rights Measurement Initiative finds that Cameroon is fulfilling 61.0% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Cameroon achieves 81.7% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 70.5% of what is expected based on the nation's level of income. Cameroon falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 30.9% of what the nation is expected to achieve based on the resources (income) it has available.

Health in Chad is suffering due to the country's weak healthcare system. Access to medical services is very limited and the health system struggles with shortage of medical staff, medicines and equipment. In 2018, the UNHCR reported that Chad currently has 615,681 people of concern, including 446,091 refugees and asylum seekers. There is a physician density of 0.04 per 1,000 population and nurse and midwife density of 0.31 per 1,000 population. The life expectancy at birth for people born in Chad, is 53 years for men and 55 years for women (2016). In 2019 Chad ranked as 187 out of 189 countries on the human development index, which places the country as a low human development country.
The Republic of Moldova has a universal health care system.

Lesotho's Human development index value for 2018 was 0.518—which put the country in the low human development category—positioning it at 164 out of 189 countries and territories. Health care services in Lesotho are delivered primarily by the government and the Christian Health Association of Lesotho. Access to health services is difficult for many people, especially in rural areas. The country's health system is challenged by the relentless increase of the burden of disease brought about by AIDS, and a lack of expertise and human resources. Serious emergencies are often referred to neighbouring South Africa. The largest contribution to mortality in Lesotho are communicable diseases, maternal, perinatal and nutritional conditions.

The quality of health in Rwanda has historically been very low, both before and immediately after the 1994 genocide. In 1998, more than one in five children died before their fifth birthday, often from malaria. But in recent years Rwanda has seen improvement on a number of key health indicators. Between 2005 and 2013, life expectancy increased from 55.2 to 64.0, under-5 mortality decreased from 106.4 to 52.0 per 1,000 live births, and incidence of tuberculosis has dropped from 101 to 69 per 100,000 people. The country's progress in healthcare has been cited by the international media and charities. The Atlantic devoted an article to "Rwanda's Historic Health Recovery". Partners In Health described the health gains "among the most dramatic the world has seen in the last 50 years".

Expenditure on health in Senegal was 4.7% of GDP in 2014, US$107 per capita.
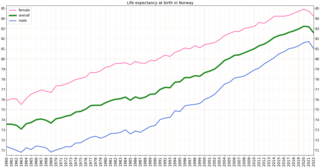
Health in Norway, with its early history of poverty and infectious diseases along with famines and epidemics, was poor for most of the population at least into the 1800s. The country eventually changed from a peasant society to an industrial one and established a public health system in 1860. Due to the high life expectancy at birth, the low under five mortality rate and the fertility rate in Norway, it is fair to say that the overall health status in the country is generally good.

Sustainable Development Goal 3, regarding "Good Health and Well-being", is one of the 17 Sustainable Development Goals established by the United Nations in 2015. The official wording is: "To ensure healthy lives and promote well-being for all at all ages." The targets of SDG 3 focus on various aspects of healthy life and healthy lifestyle. Progress towards the targets is measured using twenty-one indicators.
References
- 1 2 Skolnik, Richard L. (2021). Global health 101 (4th ed.). Burlington, MA. ISBN 978-1-284-14539-7. OCLC 1126251416.
{{cite book}}: CS1 maint: location missing publisher (link) - 1 2 3 4 Larson, C.; Mercer, A. (2004). "Global health indicators: An overview". Canadian Medical Association Journal. 171 (10): 1199–1200. doi:10.1503/cmaj.1021409. PMC 524951 . PMID 15534313.
- 1 2 3 4 5 "Health Indicators: Conceptual and Operational Considerations". Pan American Health Organization. 2022.
- 1 2 3 4 5 6 7 8 9 10 11 Development., Organisation for Economic Co-operation and (2015). Health at a Glance 2015 : OECD Indicators. OECD Publishing. ISBN 978-92-64-24351-4. OCLC 932052293.
- 1 2 3 4 5 6 7 8 Skolnik, Richard L. (2021). Global health 101 (4th ed.). Burlington, MA. ISBN 978-1-284-14539-7. OCLC 1126251416.
{{cite book}}: CS1 maint: location missing publisher (link) - 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 World Health Organization (2018). "2018 Global Reference List of 100 Core Health Indicators" (PDF). World Health Organization.
- ↑ "Activity and Mobility Promotion" (PDF). Johns Hopkins Medicine. 2022.
- 1 2 Culyer, Anthony (1978-12-31). Measuring Health: Lessons for Ontario. University of Toronto Press. doi:10.3138/9781442653412. ISBN 978-1-4426-5341-2.
- ↑ World Health Organization (2018). "2018 Global Reference List of 100 Core Health Indicators" (PDF). World Health Organization.
- 1 2 Leading Health Indicators 2030. 2020-03-05. doi:10.17226/25682. ISBN 978-0-309-67187-3. PMID 32200597. S2CID 240828832.
- ↑ "Resources on African Health and Diseases". www.africa.upenn.edu. Retrieved 2022-11-30.