Related Research Articles
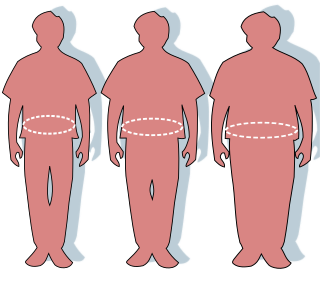
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it can potentially have negative effects on health. People are classified as obese when their body mass index (BMI)—a person's weight divided by the square of the person's height—is over 30 kg/m2; the range 25–30 kg/m2 is defined as overweight. Some East Asian countries use lower values to calculate obesity. Obesity is a major cause of disability and is correlated with various diseases and conditions, particularly cardiovascular diseases, type 2 diabetes, obstructive sleep apnea, certain types of cancer, and osteoarthritis.
Health has a variety of definitions, which have been used for different purposes over time. Health can be promoted by encouraging healthful activities, such as regular physical exercise and adequate sleep, and by reducing or avoiding unhealthful activities or situations, such as smoking or excessive stress. Some factors affecting health are due to individual choices, such as whether to engage in a high-risk behavior, while others are due to structural causes, such as whether the society is arranged in a way that makes it easier or harder for people to get necessary healthcare services. Still, other factors are beyond both individual and group choices, such as genetic disorders.

Exercise is physical activity that enhances or maintains fitness and overall health. It is performed for various reasons, including weight loss or maintenance, to aid growth and improve strength, develop muscles and the cardiovascular system, hone athletic skills, improve health, or simply for enjoyment. Many individuals choose to exercise outdoors where they can congregate in groups, socialize, and improve well-being as well as mental health.

Mental health encompasses emotional, psychological, and social well-being, influencing cognition, perception, and behavior. According to World Health Organization (WHO), it is a "state of well-being in which the individual realizes his or her abilities, can cope with the normal stresses of life, can work productively and fruitfully, and can contribute to his or her community". It likewise determines how an individual handles stress, interpersonal relationships, and decision-making. Mental health includes subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others. From the perspectives of positive psychology or holism, mental health may include an individual's ability to enjoy life and to create a balance between life activities and efforts to achieve psychological resilience. Cultural differences, personal philosophy, subjective assessments, and competing professional theories all affect how one defines "mental health". Some early signs related to mental health difficulties are sleep irritation, lack of energy, lack of appetite, thinking of harming oneself or others, self-isolating, and frequently zoning out.

Preventive healthcare, or prophylaxis, is the application of healthcare measures to prevent diseases. Disease and disability are affected by environmental factors, genetic predisposition, disease agents, and lifestyle choices, and are dynamic processes that begin before individuals realize they are affected. Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.
Health psychology is the study of psychological and behavioral processes in health, illness, and healthcare. The discipline is concerned with understanding how psychological, behavioral, and cultural factors contribute to physical health and illness. Psychological factors can affect health directly. For example, chronically occurring environmental stressors affecting the hypothalamic–pituitary–adrenal axis, cumulatively, can harm health. Behavioral factors can also affect a person's health. For example, certain behaviors can, over time, harm or enhance health. Health psychologists take a biopsychosocial approach. In other words, health psychologists understand health to be the product not only of biological processes but also of psychological, behavioral, and social processes.

A healthy diet is a diet that maintains or improves overall health. A healthy diet provides the body with essential nutrition: fluid, macronutrients such as protein, micronutrients such as vitamins, and adequate fibre and food energy.

Sedentary lifestyle is a lifestyle type, in which one is physically inactive and does little or no physical movement and/or exercise. A person living a sedentary lifestyle is often sitting or lying down while engaged in an activity like socializing, watching TV, playing video games, reading or using a mobile phone or computer for much of the day. A sedentary lifestyle contributes to poor health quality, diseases as well as many preventable causes of death.

Health education is a profession of educating people about health. Areas within this profession encompass environmental health, physical health, social health, emotional health, intellectual health, and spiritual health, as well as sexual and reproductive health education.
Workplace wellness, also known as corporate wellbeing outside the United States, is a broad term used to describe activities, programs, and/or organizational policies designed to support healthy behavior in the workplace. This often involves health education, medical screenings, weight management programs, and onsite fitness programs or facilities. It can also include flex-time for exercise, providing onsite kitchen and eating areas, offering healthy food options in vending machines, holding "walk and talk" meetings, and offering financial and other incentives for participation.
A health risk assessment is a questionnaire about a person's medical history, demographic characteristics and lifestyle. It is one of the most widely used screening tools in the field of health promotion and is often the first step in multi-component health promotion programs.

Lifestyle medicine (LM) is a branch of medicine focused on preventive healthcare and self-care dealing with prevention, research, education, and treatment of disorders caused by lifestyle factors and preventable causes of death such as nutrition, physical inactivity, chronic stress, and self-destructive behaviors including the consumption of tobacco products and drug or alcohol abuse. The goal of LM is to improve individuals' health and wellbeing by applying the 6 pillars of lifestyle medicine (nutrition, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection) to prevent chronic conditions such as cardiovascular diseases, diabetes, metabolic syndrome and obesity.
Occupational health psychology (OHP) is an interdisciplinary area of psychology that is concerned with the health and safety of workers. OHP addresses a number of major topic areas including the impact of occupational stressors on physical and mental health, the impact of involuntary unemployment on physical and mental health, work-family balance, workplace violence and other forms of mistreatment, psychosocial workplace factors that affect accident risk and safety, and interventions designed to improve and/or protect worker health. Although OHP emerged from two distinct disciplines within applied psychology, namely, health psychology and industrial and organizational psychology, for a long time the psychology establishment, including leaders of industrial/organizational psychology, rarely dealt with occupational stress and employee health, creating a need for the emergence of OHP. OHP has also been informed by other disciplines, including occupational medicine, sociology, industrial engineering, and economics, as well as preventive medicine and public health. OHP is thus concerned with the relationship of psychosocial workplace factors to the development, maintenance, and promotion of workers' health and that of their families. The World Health Organization and the International Labour Organization estimate that exposure to long working hours causes an estimated 745,000 workers to die from ischemic heart disease and stroke in 2016, mediated by occupational stress.
Health communication is the study and practice of communicating promotional health information, such as in public health campaigns, health education, and between doctor and patient. The purpose of disseminating health information is to influence personal health choices by improving health literacy. Health communication is a unique niche in healthcare that allows professionals to use communication strategies to inform and influence decisions and actions of the public to improve health.

Occupational stress is psychological stress related to one's job. Occupational stress refers to a chronic condition. Occupational stress can be managed by understanding what the stressful conditions at work are and taking steps to remediate those conditions. Occupational stress can occur when workers do not feel supported by supervisors or coworkers, feel as if they have little control over the work they perform, or find that their efforts on the job are incommensurate with the job's rewards. Occupational stress is a concern for both employees and employers because stressful job conditions are related to employees' emotional well-being, physical health, and job performance. The World Health Organization and the International Labour Organization conducted a study. The results showed that exposure to long working hours, operates through increased psycho-social occupational stress. It is the occupational risk factor with the largest attributable burden of disease, according to these official estimates causing an estimated 745,000 workers to die from ischemic heart disease and stroke events in 2016.
The Victorian Health Promotion Foundation is a statutory authority in the Australian state of Victoria, originally funded by hypothecated taxation raised by the Victorian Tobacco Act 1987. It was the first health promotion body in the world to be funded by a tax on tobacco.
Workplace health promotion is the combined efforts of employers, employees, and society to improve the mental and physical health and well-being of people at work. The term workplace health promotion denotes a comprehensive analysis and design of human and organizational work levels with the strategic aim of developing and improving health resources in an enterprise. The World Health Organization has prioritized the workplace as a setting for health promotion because of the large potential audience and influence on all spheres of a person's life. The Luxembourg Declaration provides that health and well-being of employees at work can be achieved through a combination of:

Occupational safety and health (OSH) or occupational health and safety (OHS) is a multidisciplinary field concerned with the safety, health, and welfare of people at work. OSH is related to the fields of occupational medicine and occupational hygiene and aligns with workplace health promotion initiatives. OSH also protects all the general public who may be affected by the occupational environment.
Occupational cardiovascular diseases (CVD) are diseases of the heart or blood vessels caused by working conditions, making them a form of occupational illness. These diseases include coronary heart disease, stroke, cardiomyopathy, arrythmia, and heart valve or heart chamber problems. Cardiovascular disease is the leading cause of death in the United States and worldwide. In the United States, cardiovascular diseases account for one out of four deaths. The 6th International Conference on Work Environment and Cardiovascular Diseases found that within the working age population about 10-20% of cardiovascular disease deaths can be attributed to work. Ten workplace stressors and risk factors were estimated to be associated with 120,000 U.S. deaths each year and account for 5-8% of health care costs.

Hazard controls for COVID-19 in workplaces are the application of occupational safety and health methodologies for hazard controls to the prevention of COVID-19. Vaccination is the most effective way to protect against severe illness or death from COVID-19. Multiple layers of controls are recommended, including measures such as remote work and flextime, increased ventilation, personal protective equipment (PPE) and face coverings, social distancing, and enhanced cleaning programs.
References
- ↑ Health Promotion Glossary of Terms 2021, Geneva: World Health Organization, 2021, p. 1, ISBN 9789240038349
- ↑ Participants at the 1st Global Conference on Health Promotion in Ottawa, Canada, Geneva, Switzerland: World Health Organization, 1986. Retrieved September 15, 2021.
- ↑ "Social Determinants of Health - Healthy People 2030 | health.gov". health.gov. Retrieved November 18, 2022.
- ↑ "Ottawa Charter for Health Promotion: An International Conference on Health Promotion". Public Health Agency of Canada. November 17–21, 1986. Retrieved October 28, 2023.
- ↑ Bunton R, Macdonald G (2002). Health promotion: disciplines, diversity, and developments (2nd ed.). Routledge. ISBN 978-0-415-23569-3.
- ↑ Byrd N, Białek M (2021). "Your Health vs. My Liberty: Philosophical beliefs dominated reflection and identifiable victim effects when predicting public health recommendation compliance during the COVID-19 pandemic". Cognition. 212: 104649. doi: 10.1016/j.cognition.2021.104649 . PMC 8599940 . PMID 33756152.
- 1 2 3 4 Minkler M (Spring 1989). "Health education, health promotion and the open society: an historical perspective". Health Educ Q. 16 (1): 17–30. doi:10.1177/109019818901600105. PMID 2649456. S2CID 10410928.
- ↑ Lalonde M. A new perspective on the health of Canadians. A working document. Archived May 8, 2009, at WebCite Ottawa: Government of Canada, 1974.
- ↑ Healthy people: the Surgeon General's report on health promotion and disease prevention. Archived January 31, 2009, at the Wayback Machine Washington, DC: U.S. Department of Health, Education, and Welfare, Public Health Service, Office of the Assistant Secretary for Health and Surgeon General, 1979. DHEW (PHS) Publication No. 79-55071. Retrieved February 4, 2009.
- 1 2 "A discussion document on the concept and principles of health promotion". Health Promot. 1 (1): 73–6. May 1986. doi:10.1093/heapro/1.1.73. PMID 10286854.
- 1 2 Epp J (1986). "Achieving health for all. A framework for health promotion". Health Promot. 1 (4): 419–28. doi:10.1093/heapro/1.4.419. PMID 10302169.
- 1 2 The Ottawa Charter for Health Promotion. First International Conference on Health Promotion, Ottawa, 21 November 1986. Archived March 20, 2012, at the Wayback Machine Retrieved February 4, 2009.
- ↑ Arizona State University (November 26, 2019). "Caring for family is what motivates people worldwide - International study including 27 countries shows people prioritize loved ones over everything else". EurekAlert! . Retrieved November 30, 2019.
- ↑ Ko, Ahra, et al. (2020). "Family Matters: Rethinking the Psychology of Human Social Motivation". Perspectives on Psychological Science. 15 (1): 173–201. doi: 10.1177/1745691619872986 . PMID 31791196. S2CID 208611389 . Retrieved November 30, 2019.
- ↑ "WHO | The WHO Health Promotion Glossary". WHO. Archived from the original on January 20, 2022. Retrieved August 11, 2020.
- ↑ "Healthy settings". World Health Organization (WHO) Health Promotion. October 28, 2023. Retrieved October 28, 2023.
- ↑ "About us". HPH. Retrieved October 28, 2023.
- ↑ Tones K, Tilford S (2001). Health promotion: effectiveness, efficiency and equity (3rd ed.). Cheltenham UK: Nelson Thornes. ISBN 978-0-7487-4527-2.
- ↑ European Network for Workplace Health Promotion. Workplace health promotion. Archived November 18, 2007, at the Wayback Machine Retrieved February 4, 2009.
- ↑ World Health Organization. Workplace health promotion. Benefits. Archived December 3, 2008, at the Wayback Machine Retrieved February 4, 2009.
- ↑ World Health Organization. Workplace health promotion. The workplace: a priority setting for health promotion. Archived December 4, 2008, at the Wayback Machine Retrieved February 4, 2009.
- 1 2 3 Byrne DW, Rolando LA, Aliyu MH, McGown PW, Connor LR, Awalt BM, Holmes MC, Wang L, Yarbrough MI (2016). "Modifiable Healthy Lifestyle Behaviors: 10-Year Health Outcomes From a Health Promotion Program". American Journal of Preventive Medicine. 51 (6): 1027–1037. doi:10.1016/j.amepre.2016.09.012. ISSN 1873-2607. PMID 27866595.
- 1 2 3 4 Journath G, Hammar N, Vikström M, Linnersjö A, Walldius G, Krakau I, Lindgren P, de Faire U, Hellenius ML (2020). "A Swedish primary healthcare prevention programme focusing on promotion of physical activity and a healthy lifestyle reduced cardiovascular events and mortality: 22-year follow-up of 5761 study participants and a reference group". British Journal of Sports Medicine. 54 (21): 1294–1299. doi:10.1136/bjsports-2019-101749. ISSN 1473-0480. PMC 7588408 . PMID 32680841.
- ↑ González-Dominguez ME, Romero-Sánchez JM, Ares-Camerino A, Marchena-Aparicio JC, Flores-Muñoz M, Infantes-Guzmán I, León-Asuero JM, Casals-Martín F (2017). "A Million Steps: Developing a Health Promotion Program at the Workplace to Enhance Physical Activity". Workplace Health & Safety. 65 (11): 512–516. doi: 10.1177/2165079917705146 . ISSN 2165-0969. PMID 28719762. S2CID 43473795.
- ↑ Bezzina B A, Ashton L, Watson T, James CL (2023). "Health and wellness in the Australian coal mining industry: An analysis of pre-post findings from the RESHAPE workplace health promotion program". PLOS ONE. 18 (7): e0288244. Bibcode:2023PLoSO..1888244B. doi: 10.1371/journal.pone.0288244 . ISSN 1932-6203. PMC 10328312 . PMID 37418458.
- ↑ Huang SJ, Hung WC, Shyu ML, Chou TR, Chang KC, Wai JP (2023). "Field Test of an m-Health Worksite Health Promotion Program to Increase Physical Activity in Taiwanese Employees: A Cluster-Randomized Controlled Trial". Workplace Health & Safety. 71 (1): 14–21. doi:10.1177/21650799221082304. ISSN 2165-0969. PMID 35657298. S2CID 249313373.
- ↑ Franco E, Urosa J, Barakat R, Refoyo I (March 8, 2021). "Physical Activity and Adherence to the Mediterranean Diet among Spanish Employees in a Health-Promotion Program before and during the COVID-19 Pandemic: The Sanitas-Healthy Cities Challenge". International Journal of Environmental Research and Public Health. 18 (5): 2735. doi: 10.3390/ijerph18052735 . ISSN 1660-4601. PMC 7967464 . PMID 33800372.
- ↑ Mache S, Vitzthum K, Groneberg DA, Harth V (2019). "Effects of a multi-behavioral health promotion program at worksite on smoking patterns and quit behavior". Work (Reading, Mass.). 62 (4): 543–551. doi:10.3233/WOR-192889. ISSN 1875-9270. PMID 31104040. S2CID 159039058.
- ↑ Ornek OK, Esin MN (November 4, 2020). "Effects of a work-related stress model based mental health promotion program on job stress, stress reactions and coping profiles of women workers: a control groups study". BMC Public Health. 20 (1): 1658. doi: 10.1186/s12889-020-09769-0 . ISSN 1471-2458. PMC 7641806 . PMID 33148247.
- ↑ Walker L, Smith N, Delon C (2021). "Weight loss, hypertension and mental well-being improvements during COVID-19 with a multicomponent health promotion programme on Zoom: a service evaluation in primary care". BMJ Nutrition, Prevention & Health. 4 (1): 102–110. doi:10.1136/bmjnph-2020-000219. ISSN 2516-5542. PMC 7887868 . PMID 34308117.
- ↑ Prevention Cf. "CDC - Workplace Health - Implementation - Physical Activity". www.cdc.gov. Archived from the original on October 17, 2015. Retrieved September 27, 2015.
- ↑ Engbers LH, van Poppel MN, Chin A, Paw MJ, van Mechelen W (July 2005). "Worksite health promotion programs with environmental changes: a systematic review". Am J Prev Med. 29 (1): 61–70. doi:10.1016/j.amepre.2005.03.001. PMID 15958254.
- ↑ Pelletier KR (October 2005). "A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: update VI 2000–2004". J. Occup. Environ. Med. 47 (10): 1051–8. doi:10.1097/01.jom.0000174303.85442.bf. PMID 16217246. S2CID 30828898.
- ↑ Chapman LS (2005). "Meta-evaluation of worksite health promotion economic return studies: 2005 update" (PDF). Am J Health Promot. 19 (6): 1–11. doi:10.4278/0890-1171-19.4.TAHP-1. PMID 16022209. S2CID 208067183. Archived (PDF) from the original on December 7, 2010.
- ↑ Kuoppala J, Lamminpää A, Husman P (November 2008). "Work health promotion, job well-being, and sickness absences—a systematic review and meta-analysis". J. Occup. Environ. Med. 50 (11): 1216–27. doi:10.1097/JOM.0b013e31818dbf92. PMID 19001948. S2CID 7330866.
- ↑ Martin A, Sanderson K, Cocker F (January 2009). "Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms". Scand J Work Environ Health. 35 (1): 7–18. doi: 10.5271/sjweh.1295 . PMID 19065280.
- ↑ Goetzel RZ, Ozminkowski RJ (2008). "The health and cost benefits of work site health-promotion programs". Annu Rev Public Health. 29: 303–23. doi: 10.1146/annurev.publhealth.29.020907.090930 . PMID 18173386.
- ↑ Pega F, Nafradi B, Momen N, Ujita Y, Streicher K, Prüss-Üstün A, Technical Advisory Group (2021). "Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000–2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury". Environment International. 154: 106595. doi: 10.1016/j.envint.2021.106595 . PMC 8204267 . PMID 34011457.