The Ministry of Health is the public service department of New Zealand responsible for healthcare in New Zealand. It came into existence in its current form in 1993.
District health boards (DHBs) in New Zealand were organisations established by the New Zealand Public Health and Disability Act 2000 under the Fifth Labour Government, responsible for ensuring the provision of health and disability services to populations within a defined geographical area. They existed from 1 January 2001, when the Act came into force, to 30 June 2022. Initially there were 21 DHBs, and this was reduced to 20 organisations in 2010: fifteen in the North Island and five in the South Island. DHBs received public funding from the Ministry of Health on behalf of the Crown, based on a formula that took into account the total number, gender, age, socio-economic status and ethnic mix of their population. DHBs were governed by boards, which were partially elected and partially appointed by the minister of Health.
District Nurses work manage care within the community and lead teams of community nurses and support workers. The role requires registered nurses to take a NMC approved specialist practitioner course. Duties generally include visiting house-bound patients and providing advice and care such as palliative care, wound management, catheter and continence care and medication support. Their work involves both follow-up care for recently discharged hospital inpatients and longer-term care for chronically ill patients who may be referred by many other services, as well as working collaboratively with general practitioners in preventing unnecessary or avoidable hospital admissions.

Auckland City Hospital is a public hospital located in Grafton, Auckland, New Zealand. It is the largest hospital in New Zealand, as well as one of the oldest medical facilities in the country. It provides a total of 1,165 beds. It was established in 2003 as an amalgam of Auckland Hospital, Starship Hospital, Green Lane Hospital and National Women's Hospital. Public hospitals in Auckland have been run by Te Whatu Ora – Health New Zealand since 2022.
A formulary is a list of pharmaceutical drugs, often decided upon by a group of people, for various reasons such as insurance coverage or use at a medical facility. Traditionally, a formulary contained a collection of formulas for the compounding and testing of medication. Today, the main function of a prescription formulary is to specify particular medications that are approved to be prescribed at a particular hospital, in a particular health system, or under a particular health insurance policy. The development of prescription formularies is based on evaluations of efficacy, safety, and cost-effectiveness of drugs.
The Pharmaceutical Management Agency, better known as Pharmac, is a New Zealand Crown entity that decides, on behalf of Te Whatu Ora – Health New Zealand, which medicines and pharmaceutical products are subsidised for use in the community and public hospitals.

Christchurch Hospital is the largest tertiary hospital in the South Island of New Zealand. The public hospital is in the centre of Christchurch city, on the edge of Hagley Park, and serves the wider Canterbury region. The Canterbury District Health Board (CDHB) operates the hospital with funding from the government.

Auckland District Health Board (ADHB) was a district health board that provided healthcare in the Auckland Region in New Zealand, mainly on the Auckland isthmus. This district health board existed between 2001 and 2022 and was governed by a part-elected, part-appointed board. In 2022, its functions and responsibilities were subsumed by Te Whatu Ora and Te Aka Whai Ora.
Contraceptive rights in New Zealand are extensive. There are many options available to women seeking contraception. There are also options for men. Government funding keeps the cost of most types of contraception low in most cases. Family planning options in New Zealand are generally in keeping with the United Nations stance towards sexual and reproductive rights although the country has received criticism in some aspects.

The South Canterbury District Health Board was a district health board with the focus on providing healthcare to the Timaru, Mackenzie, Waimate districts in New Zealand. In July 2022, it was merged into the national health service Te Whatu Ora.

The Canterbury District Health Board was a district health board with the focus on providing healthcare to the Canterbury region of New Zealand, north of the Rangitata River. It was responsible for roughly 579,000 residents, or 12% of New Zealand's population. The Canterbury District Health Board covered a territory of 26,881 square kilometers and was divided between six territorial local authorities. In July 2022, the Canterbury DHB was merged into the national health service Te Whatu Ora.

The Capital and Coast District Health Board (CCDHB) was a district health board with the focus on providing healthcare to Wellington City, Porirua City and the Kāpiti Coast in New Zealand. The CCDHB employed about 6000 people across the Wellington Region. It was disestablished on 1 July 2022, with its functions and responsibilities being taken over by the national health service Te Whatu Ora.

Mental health in New Zealand generally follows the trends of mental health in other OECD countries. New Zealand's 'outdoor life style' and high standard of living are balanced by isolation and a self-reliant culture, which discourages asking for help. Historically, people with mental health problems were institutionalised, whereas now the focus is on care in the wider community. The stigma around poor mental health has been lessened in recent years as a result of this change and public education campaigns. However, New Zealand's minorities and youth continue to be over-represented in the negative mental health statistics.

MidCentral District Health Board was a district health board that provided healthcare in the Manawatū region of New Zealand. The DHB covers the Manawatū District, Palmerston North City, Tararua District, Horowhenua District, and the Ōtaki ward of the Kāpiti Coast District. In July 2022, the MidCentral DHB was merged into the national health service Te Whatu Ora.

The Northland District Health Board is a district health board with the focus on providing healthcare to the Northland Region of New Zealand. In July 2022, the Northland DHB was merged into the national health service Te Whatu Ora.

The Southern District Health Board was a district health board which provided healthcare to an area covering the southern half of the South Island of New Zealand. In July 2022, the Southern DHB was dissolved as part of a nationwide overhaul of the district health board system. Its former functions and responsibilities were taken over by Te Whatu Ora.

The Tairāwhiti District Health Board, branded as Hauora Tairāwhiti since 2015, was a district health board with the focus on providing healthcare to the Gisborne District of New Zealand. In July 2022, the Tairāwhiti DHB was merged into the national health service Te Whatu Ora.

The Waikato District Health Board was a district health board that provided healthcare to the Waikato region of New Zealand.
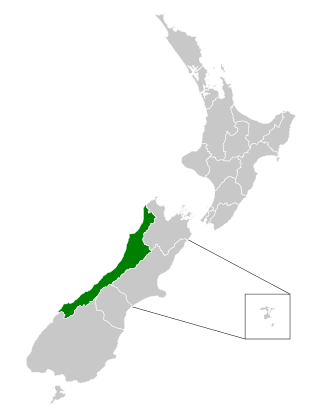
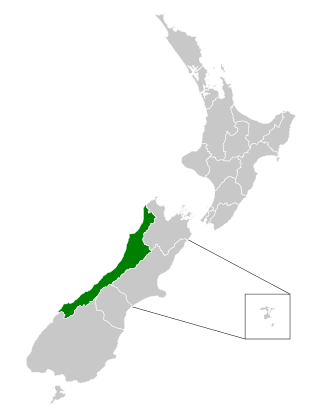
The West Coast District Health Board was a district health board with the focus on providing healthcare to the West Coast region of New Zealand. In July 2022, the West Coast DHB's functions and responsibilities were taken over by the national health service Te Whatu Ora.
Te Whatu Ora Health New Zealand is a public health agency established by the New Zealand Government to replace the country's 20 district health boards (DHBs) on 1 July 2022. Te Whatu Ora is charged with working alongside the Public Health Agency and Te Aka Whai Ora to manage the provision of healthcare services in New Zealand. Margie Apa was appointed chief executive of Te Whatu Ora in December 2021.