Related Research Articles
A transient ischemic attack (TIA), commonly known as a mini-stroke, is a minor stroke whose noticeable symptoms usually end in less than an hour. TIA causes the same symptoms associated with strokes, such as weakness or numbness on one side of the body, sudden dimming or loss of vision, difficulty speaking or understanding language, slurred speech, or confusion.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.

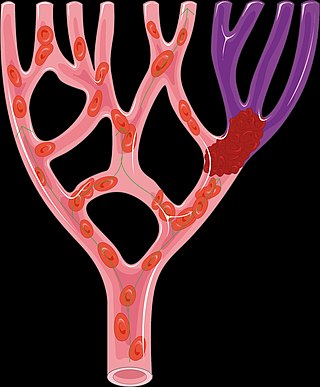
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.
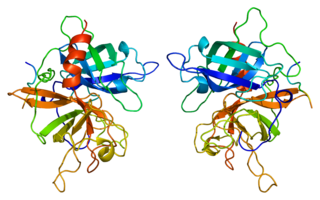
Tissue-type plasminogen activator, short name tPA, is a protein that facilitates the breakdown of blood clots. It acts as an enzyme to convert plasminogen into its active form plasmin, the major enzyme responsible for clot breakdown. It is a serine protease found on endothelial cells lining the blood vessels. Human tPA is encoded by the PLAT gene, and has a molecular weight of ~70 kDa in the single-chain form.

Stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functioning properly.

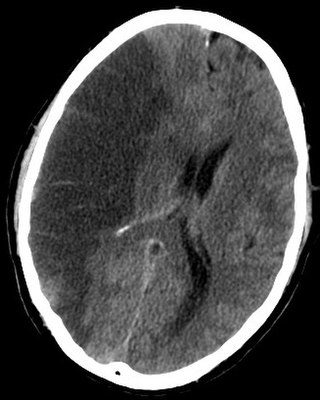
Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.
Alteplase, sold under the brand name Activase among others, is a biosynthetic form of human tissue-type plasminogen activator (t-PA). It is a thrombolytic medication used to treat acute ischemic stroke, acute ST-elevation myocardial infarction, pulmonary embolism associated with low blood pressure, and blocked central venous catheter. It is given by injection into a vein or artery. Alteplase is the same as the normal human plasminogen activator produced in vascular endothelial cells and is synthesized via recombinant DNA technology in Chinese hamster ovary cells (CHO). Alteplase causes the breakdown of a clot by inducing fibrinolysis.

Desmoteplase is a novel, highly fibrin-specific "clot-busting" (thrombolytic) drug in development that reached phase III clinical trials. The Danish pharmaceutical company, Lundbeck, owns the worldwide rights to Desmoteplase. In 2009, two large trials were started to test it as a safe and effective treatment for patients with acute ischaemic stroke. After disappointing results in DIAS-3, DIAS-4 was terminated, and in December 2014 Lundbeck announced that they would stop the development of desmoteplase.

Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.

Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).

Cerebral infarction is the pathologic process that results in an area of necrotic tissue in the brain. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia), most commonly due to thromboembolism, and manifests clinically as ischemic stroke. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.
Brain ischemia is a condition in which there is insufficient bloodflow to the brain to meet metabolic demand. This leads to poor oxygen supply or cerebral hypoxia and thus leads to the death of brain tissue or cerebral infarction/ischemic stroke. It is a sub-type of stroke along with subarachnoid hemorrhage and intracerebral hemorrhage.
Hypertensive encephalopathy (HE) is general brain dysfunction due to significantly high blood pressure. Symptoms may include headache, vomiting, trouble with balance, and confusion. Onset is generally sudden. Complications can include seizures, posterior reversible encephalopathy syndrome, and bleeding in the back of the eye.

Vertebral artery dissection (VAD) is a flap-like tear of the inner lining of the vertebral artery, which is located in the neck and supplies blood to the brain. After the tear, blood enters the arterial wall and forms a blood clot, thickening the artery wall and often impeding blood flow. The symptoms of vertebral artery dissection include head and neck pain and intermittent or permanent stroke symptoms such as difficulty speaking, impaired coordination, and visual loss. It is usually diagnosed with a contrast-enhanced CT or MRI scan.
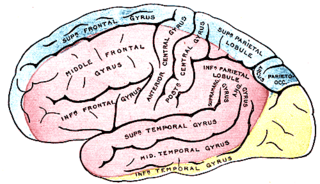
Anterior cerebral artery syndrome is a condition whereby the blood supply from the anterior cerebral artery (ACA) is restricted, leading to a reduction of the function of the portions of the brain supplied by that vessel: the medial aspects of the frontal and parietal lobes, basal ganglia, anterior fornix and anterior corpus callosum.
Leukostasis is a medical emergency most commonly seen in patients with acute myeloid leukemia. It is characterized by an extremely elevated blast cell count and symptoms of decreased tissue perfusion. The pathophysiology of leukostasis is not well understood, but inadequate delivery of oxygen to the body's cells is the result. Leukostasis is diagnosed when white cell plugs are seen in the microvasculature. The most common symptoms are dyspnea and hypoxia, usually accompanied by visual changes, headaches, dizziness, confusion, somnolence, and coma. Prompt treatment is required since, if left untreated, it has a very high mortality rate. Treatments aim to rapidly reduce white blood cell counts while also treating the underlying disorder.

Repinotan (BAYx3702), an aminomethylchroman derivative, is a selective 5-HT1A receptor full agonist with high potency and efficacy. It has neuroprotective effects in animal studies, and was trialed in humans for reducing brain injury following head trauma. It was subsequently trialed up to phase II for treatment of stroke, but while side effects were mild and consisted mainly of nausea, repinotan failed to demonstrate sufficient efficacy to justify further clinical trials. However, repinotan continues to be investigated for other applications, and was found to be effective at counteracting the respiratory depression produced by morphine, though with slight reduction in analgesic effects.
Very low cerebral blood volume (VLCBV) is a measurement of hemorrhagic transformation degree in the tissue surrounding the lesion in strokes. It is counted as one of the penumbral imaging procedures along with less commonly used methods such as diffusion-weighted imaging (DWI). These are used to predict if there is going to be a hemorrhage after the treatment by tPA. In advanced centers, this measurement helps with using tPA beyond the standard time limit without risk of hemorrhage.
Perinatal stroke is a disease where an infant has a stroke between the 140th day of the gestation period and the 28th postpartum day, affecting up to 1 in 2300 live births. This disease is further divided into three subgroups, namely neonatal arterial ischemic stroke, neonatal cerebral sinovenous ischemic stroke, and presumed perinatal stroke. Several risk factors contribute to perinatal stroke including birth trauma, placental abruption, infections, and the mother's health.
References
- 1 2 Gaillard F. "Hemorrhagic transformation of ischemic infarct". Radiology Reference Article. Radiopaedia. Retrieved 2023-02-28.
- ↑ The NINDS t-PA Stroke Study Group (November 1997). "Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke". Stroke. 28 (11): 2109–18. doi: 10.1161/01.str.28.11.2109 . PMID 9368550.
- 1 2 3 Spronk E, Sykes G, Falcione S, Munsterman D, Joy T, Kamtchum-Tatuene J, Jickling GC (2021). "Hemorrhagic Transformation in Ischemic Stroke and the Role of Inflammation". Frontiers in Neurology. 12: 661955. doi: 10.3389/fneur.2021.661955 . PMC 8160112 . PMID 34054705.
- ↑ Marsh EB, Llinas RH, Schneider AL, Hillis AE, Lawrence E, Dziedzic P, Gottesman RF (January 2016). "Predicting Hemorrhagic Transformation of Acute Ischemic Stroke: Prospective Validation of the HeRS Score". Medicine. 95 (2): e2430. doi:10.1097/MD.0000000000002430. PMC 4718251 . PMID 26765425.
- ↑ Yaghi S, Willey JZ, Cucchiara B, Goldstein JN, Gonzales NR, Khatri P, et al. (December 2017). "Treatment and Outcome of Hemorrhagic Transformation After Intravenous Alteplase in Acute Ischemic Stroke: A Scientific Statement for Healthcare Professionals From the American Heart Association/American Stroke Association". Stroke. 48 (12): e343–e361. doi: 10.1161/STR.0000000000000152 . PMID 29097489. S2CID 3779945.
- 1 2 Hong JM, Kim DS, Kim M (2021). "Hemorrhagic Transformation After Ischemic Stroke: Mechanisms and Management". Frontiers in Neurology. 12: 703258. doi: 10.3389/fneur.2021.703258 . PMC 8669478 . PMID 34917010.
- 1 2 Stone JA, Willey JZ, Keyrouz S, Butera J, McTaggart RA, Cutting S, et al. (January 2017). "Therapies for Hemorrhagic Transformation in Acute Ischemic Stroke". Current Treatment Options in Neurology. 19 (1): 1. doi:10.1007/s11940-017-0438-5. PMID 28130682. S2CID 3294843.
- ↑ Unnithan AK, Das J, Mehta P (2022). "Hemorrhagic Stroke". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32644599 . Retrieved 2023-02-28.