Health informatics is the field of science and engineering that aims at developing methods and technologies for the acquisition, processing, and study of patient data, which can come from different sources and modalities, such as electronic health records, diagnostic test results, medical scans. The health domain provides an extremely wide variety of problems that can be tackled using computational techniques.

Preventive healthcare, or prophylaxis, consists of measures taken for the purposes of disease prevention. Disease and disability are affected by environmental factors, genetic predisposition, disease agents, and lifestyle choices, and are dynamic processes which begin before individuals realize they are affected. Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.

An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.
The cancer Biomedical Informatics Grid (caBIG) was a US government program to develop an open-source, open access information network called caGrid for secure data exchange on cancer research. The initiative was developed by the National Cancer Institute and was maintained by the Center for Biomedical Informatics and Information Technology (CBIIT). In 2011 a report on caBIG raised significant questions about effectiveness and oversight, and its budget and scope were significantly trimmed. In May 2012, the National Cancer Informatics Program (NCIP) was created as caBIG's successor program.
A Regional Health Information Organization, also called a Health Information Exchange Organization, is a multistakeholder organization created to facilitate a health information exchange (HIE) – the transfer of healthcare information electronically across organizations – among stakeholders of that region's healthcare system. The ultimate objective is to improve the safety, quality, and efficiency of healthcare as well as access to healthcare through the efficient application of health information technology. RHIOs are also intended to support secondary use of clinical data for research as well as institution/provider quality assessment and improvement. RHIO stakeholders include smaller clinics, hospitals, medical societies, major employers and payers.
A Patient Safety Organization (PSO) is a group, institution, or association that improves medical care by reducing medical errors. Common functions of patient safety organizations are data collection and analysis, reporting, education, funding, and advocacy. A PSO differs from a Federally designed Patient Safety Organization (PSO), which provides health care providers in the U.S. privilege and confidentiality protections for efforts to improve patient safety and the quality of patient care delivery
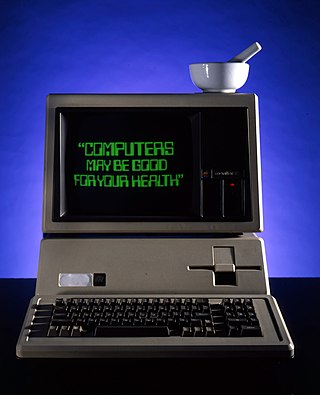
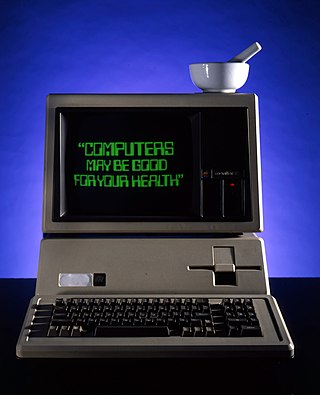
Health information technology (HIT) is health technology, particularly information technology, applied to health and health care. It supports health information management across computerized systems and the secure exchange of health information between consumers, providers, payers, and quality monitors. Based on a 2008 report on a small series of studies conducted at four sites that provide ambulatory care – three U.S. medical centers and one in the Netherlands, the use of electronic health records (EHRs) was viewed as the most promising tool for improving the overall quality, safety and efficiency of the health delivery system.
In economics, supplier induced demand (SID) may occur when asymmetry of information exists between supplier and consumer. The supplier can use superior information to encourage an individual to demand a greater quantity of the good or service they supply than the Pareto efficient level, should asymmetric information not exist. The result of this is a welfare loss.
Connected health is a socio-technical model for healthcare management and delivery by using technology to provide healthcare services remotely. Connected health, also known as technology enabled care (TEC) aims to maximize healthcare resources and provide increased, flexible opportunities for consumers to engage with clinicians and better self-manage their care. It uses readily available consumer technologies to deliver patient care outside of the hospital or doctor's office. Connected health encompasses programs in telehealth, remote care and disease and lifestyle management, often leverages existing technologies such as connected devices using cellular networks and is associated with efforts to improve chronic care. However, there is an increasing blur between software capabilities and healthcare needs whereby technologists are now providing the solutions to support consumer wellness and provide the connectivity between patient data, information and decisions. This calls for new techniques to guide Connected Health solutions such as "design thinking" to support software developers in clearly identifying healthcare requirements, and extend and enrich traditional software requirements gathering techniques.
Health communication is the study and practice of communicating promotional health information, such as in public health campaigns, health education, and between doctor and patient. The purpose of disseminating health information is to influence personal health choices by improving health literacy. Health communication is a unique niche in healthcare that allows professionals to use communication strategies to inform and influence decisions and actions of the public to improve health.
Comparative effectiveness research (CER) is the direct comparison of existing health care interventions to determine which work best for which patients and which pose the greatest benefits and harms. The core question of comparative effectiveness research is which treatment works best, for whom, and under what circumstances. Engaging various stakeholders in this process, while difficult, makes research more applicable through providing information that improves patient decision making.
AcademyHealth is a nonpartisan, nonprofit professional organization dedicated to advancing the fields of health services research and health policy. It is a professional organization for health services researchers, health policy analysts, and health practitioners, and it is a nonpartisan source for health research and policy. The organization was founded in 2000, in a merger between the Alpha Center and the Association for Health Services Research (AHSR). In 2008, the organization had approximately 4000 health services researcher members.
Digital health is a discipline that includes digital care programs, technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and to make medicine more personalized and precise. It uses information and communication technologies to facilitate understanding of health problems and challenges faced by people receiving medical treatment and social prescribing in more personalised and precise ways. The definitions of digital health and its remits overlap in many ways with those of health and medical informatics.
Health care quality is a level of value provided by any health care resource, as determined by some measurement. As with quality in other fields, it is an assessment of whether something is good enough and whether it is suitable for its purpose. The goal of health care is to provide medical resources of high quality to all who need them; that is, to ensure good quality of life, cure illnesses when possible, to extend life expectancy, and so on. Researchers use a variety of quality measures to attempt to determine health care quality, including counts of a therapy's reduction or lessening of diseases identified by medical diagnosis, a decrease in the number of risk factors which people have following preventive care, or a survey of health indicators in a population who are accessing certain kinds of care.
Health information on the Internet refers to all health-related information communicated through or available on the Internet.
Grid-Enabled Measures (GEM) is an initiative of the National Institutes of Health (NIH) National Cancer Institute (NCI). GEM is a web-based collaborative platform and database enabling researchers to exchange harmonized data about behavioral constructs, measures, and datasets.
Health care analytics is the health care analysis activities that can be undertaken as a result of data collected from four areas within healthcare; claims and cost data, pharmaceutical and research and development (R&D) data, clinical data, and patient behavior and sentiment data (patient behaviors and preferences,. Health care analytics is a growing industry in the United States, expected to grow to more than $31 billion by 2022. The industry focuses on the areas of clinical analysis, financial analysis, supply chain analysis, as well as marketing, fraud and HR analysis.

Dipak Kalra is President of the European Institute for Health Records and of the European Institute for Innovation through Health Data. He undertakes international research and standards development, and advises on adoption strategies, relating to Electronic Health Records.
Health data is any data "related to health conditions, reproductive outcomes, causes of death, and quality of life" for an individual or population. Health data includes clinical metrics along with environmental, socioeconomic, and behavioral information pertinent to health and wellness. A plurality of health data are collected and used when individuals interact with health care systems. This data, collected by health care providers, typically includes a record of services received, conditions of those services, and clinical outcomes or information concerning those services. Historically, most health data has been sourced from this framework. The advent of eHealth and advances in health information technology, however, have expanded the collection and use of health data—but have also engendered new security, privacy, and ethical concerns. The increasing collection and use of health data by patients is a major component of digital health.
Learning health systems (LHS) are healthcare systems in which knowledge generation processes are embedded in daily practice to improve healthcare. At its most fundamental level, a learning health system applies a conceptual approach wherein science, informatics, incentives, and culture are aligned to support continuous improvement, innovation, and equity, and seamlessly embed knowledge and best practices into care delivery