Related Research Articles
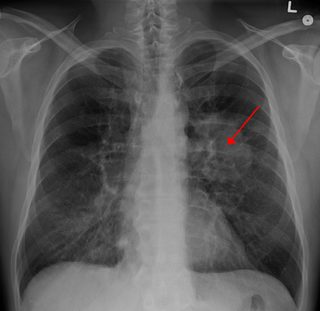
Lung cancer, also known as lung carcinoma, since about 98–99% of all lung cancers are carcinomas, is a malignant lung tumor characterized by uncontrolled cell growth in tissues of the lung. Lung carcinomas derive from transformed, malignant cells that originate as epithelial cells, or from tissues composed of epithelial cells. Other lung cancers, such as the rare sarcomas of the lung, are generated by the malignant transformation of connective tissues, which arise from mesenchymal cells. Lymphomas and melanomas can also rarely result in lung cancer.

Liver transplantation or hepatic transplantation is the replacement of a diseased liver with the healthy liver from another person (allograft). Liver transplantation is a treatment option for end-stage liver disease and acute liver failure, although availability of donor organs is a major limitation. The most common technique is orthotopic transplantation, in which the native liver is removed and replaced by the donor organ in the same anatomic position as the original liver. The surgical procedure is complex, requiring careful harvest of the donor organ and meticulous implantation into the recipient. Liver transplantation is highly regulated, and only performed at designated transplant medical centers by highly trained transplant physicians and supporting medical team. The duration of the surgery ranges from 4 to 18 hours depending on outcome. Favorable outcomes require careful screening for eligible recipient, as well as a well-calibrated live or cadaveric donor match.

Malignancy is the tendency of a medical condition to become progressively worse.

Cardiothoracic surgery is the field of medicine involved in surgical treatment of organs inside the thoracic cavity — generally treatment of conditions of the heart, lungs, and other pleural or mediastinal structures.

Lung transplantation, or pulmonary transplantation, is a surgical procedure in which one or both lungs are replaced by lungs from a donor. Donor lungs can be retrieved from a living or deceased donor. A living donor can only donate one lung lobe. With some lung diseases, a recipient may only need to receive a single lung. With other lung diseases such as cystic fibrosis, it is imperative that a recipient receive two lungs. While lung transplants carry certain associated risks, they can also extend life expectancy and enhance the quality of life for those with end stage pulmonary disease.
Mark A. Hardy is Auchincloss Professor of Surgery, Director Emeritus of the Transplant Centre, and Vice Chairman and Residency Program Director of the Department of Surgery at the Columbia University College of Physicians and Surgeons and NewYork-Presbyterian Hospital in New York City.
Joel D. Cooper, F.A.C.S., a thoracic surgeon, is known for having completed the first successful lung transplant and the first successful double lung transplant.
Norman Edward Shumway was a pioneer of heart surgery at Stanford University. He was the 67th president of the American Association for Thoracic Surgery and the first to perform an adult human to human heart transplantation in the United States.

A heart transplant, or a cardiac transplant, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease when other medical or surgical treatments have failed. As of 2018, the most common procedure is to take a functioning heart, with or without both lungs, from a recently deceased organ donor and implant it into the patient. The patient's own heart is either removed and replaced with the donor heart or, much less commonly, the recipient's diseased heart is left in place to support the donor heart.
Raja Michael Flores, M.D., is an American thoracic surgeon and former candidate for mayor of New York City, currently Chief of the Division of Thoracic Surgery at Mount Sinai Hospital and Ames Professor of Cardiothoracic Surgery at the Icahn School of Medicine at Mount Sinai, both in New York City. On March 20, 2021, Dr. Flores announced his campaign for mayor of NYC.
ABO-incompatible (ABOi) transplantation is a method of allocation in organ transplantation that permits more efficient use of available organs regardless of ABO blood type, which would otherwise be unavailable due to hyperacute rejection. Primarily in use in infants and young toddlers, research is ongoing to allow for increased use of this capability in adult transplants. Normal ABO-compatibility rules may be observed for all recipients. This means that anyone may receive a transplant of a type-O organ, and consequently, type-O recipients are one of the biggest beneficiaries of ABO-incompatible transplants. While focus has been on infant heart transplants, the principles generally apply to other forms of solid organ transplantation.
Hyperthermic intrathoracic chemotherapy (HITOC) is part of a surgical strategy employed in the treatment of various pleural malignancies. The pleura in this situation could be considered to include the surface linings of the chest wall, lungs, mediastinum, and diaphragm. HITOC is the chest counterpart of HIPEC. Traditionally used in the treatment of malignant mesothelioma, a primary malignancy of the pleura, this modality has recently been evaluated in the treatment of secondary pleural malignancies.

Shaf Keshavjee is a Canadian surgeon and the current Surgeon-in-Chief at University Health Network in Toronto, the Director of the Toronto Lung Transplant Program, as well as a clinical scientist and professor with the University of Toronto.

Stuart William Jamieson is a British cardiothoracic surgeon, specialising in pulmonary thromboendarterectomy (PTE), a surgical procedure performed to remove organized clotted blood (thrombus) from pulmonary arteries in people with chronic thromboembolic pulmonary hypertension (CTEPH).
Jack Greene Copeland is an American cardiothoracic surgeon, who has established procedures in heart transplantation including repeat heart transplantation, the implantation of total artificial hearts (TAH) to bridge the time to heart transplant, innovations in left ventricular assist devices (LVAD) and the technique of "piggybacking" a second heart in a person, while leaving them the original.
Edward B. Stinson is an American retired cardiothoracic surgeon living in Los Altos, United States, who assisted Norman Shumway in America's first adult human-to-human heart transplantation on 6 January 1968 at Stanford University.
Eric A. Rose is an American cardiothoracic surgeon, scientist, entrepreneur and professor and Chairman of the Department of Population Health Science & Policy, and Associate Director for Clinical Outcomes at Mount Sinai Heart. He is best known for performing the first successful paediatric heart transplant, in 1984 while at NewYork–Presbyterian Hospital (NYP).

Keith Reemtsma was an American transplant surgeon, best known for the cross-species kidney transplantation operation from chimpanzee to human in 1964. With only the early immunosuppressants and no long-term dialysis, the female recipient survived nine months, long enough to return to work.

Limited-stage small cell lung carcinoma (LS-SCLC) is a type of small cell lung cancer (SCLC) that is confined to an area which is small enough to be encompassed within a radiation portal. This generally includes cancer to one side of the lung and those might have reached the lymph nodes on the same side of the lung. 33% patients with small cell lung cancer are diagnosed with limited-stage small cell lung carcinoma when it is first found. Common symptoms include but are not limited to persistent cough, chest pain, rust-coloured sputum, shortness of breath, fatigue, weight loss, wheezing, hoarseness and recurrent respiratory tract infections such as pneumonia and bronchitis. Nervous system problems, Cushing syndrome and SIADH can also be associated with small cell lung cancer. Unlike extensive-stage small cell lung cancer, limited-stage small cell lung carcinoma is potentially curable. Standard treatments consist of surgery, platinum-based combination chemotherapy, thoracic irradiation, and prophylactic cranial irradiation. Patient five-year survival rate has significantly increased from 1% with surgery to 26% after the application of combination chemotherapy.
Gaetano Ciancio is an Italian American surgeon at the University of Miami who specializes in kidney transplant. He is the chief medical and academic officer of the Miami Transplant Institute and the director of its Kidney & Kidney-Pancreas Programs. His most significant contributions to medicine are related to surgically treating kidney cancer once it has spread to the inferior vena cava and in optimizing the immunosuppression protocol after kidney transplant.
References
- ↑ "Living Donor Liver Transplantation Saves Lives". Columbia University Department of Surgery. Archived from the original on September 27, 2007.
- ↑ "Extended Donor Criteria for Transplantation: Saving Lives by Increasing Alternatives". Columbia University Department of Surgery. Archived from the original on June 15, 2006.
- ↑ "Lung Transplant Surgery". Columbia University Department of Surgery. Archived from the original on April 27, 2007. Retrieved 11 May 2020.
- ↑ Altman, Lawrence K. (11 March 2005). "Clinton's 4-Hour Surgery Went Well, Doctors Say". The New York Times. Retrieved 11 May 2020.
- ↑ "Dr. Sonett Receives Humanitarian Award". Columbia University Department of Surgery. Archived from the original on September 26, 2007.