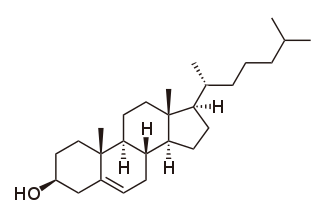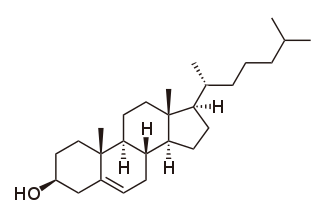
Cholesterol is the principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils.
High-density lipoprotein (HDL) is one of the five major groups of lipoproteins. Lipoproteins are complex particles composed of multiple proteins which transport all fat molecules (lipids) around the body within the water outside cells. They are typically composed of 80–100 proteins per particle. HDL particles enlarge while circulating in the blood, aggregating more fat molecules and transporting up to hundreds of fat molecules per particle.

Low-density lipoprotein (LDL) is one of the five major groups of lipoprotein that transport all fat molecules around the body in extracellular water. These groups, from least dense to most dense, are chylomicrons, very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), low-density lipoprotein (LDL) and high-density lipoprotein (HDL). LDL delivers fat molecules to cells. LDL is involved in atherosclerosis, a process in which it is oxidized within the walls of arteries.

A lipoprotein is a biochemical assembly whose primary function is to transport hydrophobic lipid molecules in water, as in blood plasma or other extracellular fluids. They consist of a triglyceride and cholesterol center, surrounded by a phospholipid outer shell, with the hydrophilic portions oriented outward toward the surrounding water and lipophilic portions oriented inward toward the lipid center. A special kind of protein, called apolipoprotein, is embedded in the outer shell, both stabilising the complex and giving it a functional identity that determines its role.
Lipid-lowering agents, also sometimes referred to as hypolipidemic agents, cholesterol-lowering drugs, or antihyperlipidemic agents are a diverse group of pharmaceuticals that are used to lower the level of lipids and lipoproteins such as cholesterol, in the blood (hyperlipidemia). The American Heart Association recommends the descriptor 'lipid lowering agent' be used for this class of drugs rather than the term 'hypolipidemic'.

In pharmacology, the fibrates are a class of amphipathic carboxylic acids and esters. They are derivatives of fibric acid. They are used for a range of metabolic disorders, mainly hypercholesterolemia, and are therefore hypolipidemic agents.
Very-low-density lipoprotein (VLDL), density relative to extracellular water, is a type of lipoprotein made by the liver. VLDL is one of the five major groups of lipoproteins that enable fats and cholesterol to move within the water-based solution of the bloodstream. VLDL is assembled in the liver from triglycerides, cholesterol, and apolipoproteins. VLDL is converted in the bloodstream to low-density lipoprotein (LDL) and intermediate-density lipoprotein (IDL). VLDL particles have a diameter of 30–80 nm. VLDL transports endogenous products, whereas chylomicrons transport exogenous (dietary) products. In the early 2010s both the lipid composition and protein composition of this lipoprotein were characterised in great detail.

Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood. It is a form of hyperlipidemia, hyperlipoproteinemia, and dyslipidemia.
Dyslipidemia is a metabolic disorder characterized by abnormally high or low amounts of any or all lipids or lipoproteins in the blood. Dyslipidemia is a risk factor for the development of atherosclerotic cardiovascular diseases (ASCVD), which include coronary artery disease, cerebrovascular disease, and peripheral artery disease. Although dyslipidemia is a risk factor for ASCVD, abnormal levels don't mean that lipid lowering agents need to be started. Other factors, such as comorbid conditions and lifestyle in addition to dyslipidemia, is considered in a cardiovascular risk assessment. In developed countries, most dyslipidemias are hyperlipidemias; that is, an elevation of lipids in the blood. This is often due to diet and lifestyle. Prolonged elevation of insulin resistance can also lead to dyslipidemia. Likewise, increased levels of O-GlcNAc transferase (OGT) may cause dyslipidemia.

Combined hyperlipidemia is a commonly occurring form of hypercholesterolemia characterised by increased LDL and triglyceride concentrations, often accompanied by decreased HDL. On lipoprotein electrophoresis it shows as a hyperlipoproteinemia type IIB. It is the most commonly inherited lipid disorder, occurring in around one in 200 persons. In fact, almost one in five individuals who develop coronary heart disease before the age of 60 have this disorder.

Gemfibrozil, sold under the brand name Lopid among others, is a medication used to treat abnormal blood lipid levels. It is generally less preferred than statins. Use is recommended together with dietary changes and exercise. It is unclear if it changes the risk of heart disease. It is taken by mouth.
Intermediate-density lipoproteins (IDLs) belong to the lipoprotein particle family and are formed from the degradation of very low-density lipoproteins as well as high-density lipoproteins. IDL is one of the five major groups of lipoproteins that enable fats and cholesterol to move within the water-based solution of the bloodstream. Each native IDL particle consists of protein that encircles various lipids, enabling, as a water-soluble particle, these lipids to travel in the aqueous blood environment as part of the fat transport system within the body. Their size is, in general, 25 to 35 nm in diameter, and they contain primarily a range of triglycerides and cholesterol esters. They are cleared from the plasma into the liver by receptor-mediated endocytosis, or further degraded by hepatic lipase to form LDL particles.

Apolipoproteins are proteins that bind lipids to form lipoproteins. They transport lipids in blood, cerebrospinal fluid and lymph.
Hyperlipidemia is abnormally high levels of any or all lipids or lipoproteins in the blood. The term hyperlipidemia refers to the laboratory finding itself and is also used as an umbrella term covering any of various acquired or genetic disorders that result in that finding. Hyperlipidemia represents a subset of dyslipidemia and a superset of hypercholesterolemia. Hyperlipidemia is usually chronic and requires ongoing medication to control blood lipid levels.

Familial hypercholesterolemia (FH) is a genetic disorder characterized by high cholesterol levels, specifically very high levels of low-density lipoprotein cholesterol, in the blood and early cardiovascular diseases. The most common mutations diminish the number of functional LDL receptors in the liver or produce abnormal LDL receptors that never go to the cell surface to function properly. Since the underlying body biochemistry is slightly different in individuals with FH, their high cholesterol levels are less responsive to the kinds of cholesterol control methods which are usually more effective in people without FH. Nevertheless, treatment is usually effective.
Lecithin cholesterol acyltransferase deficiency is a disorder of lipoprotein metabolism. The disease has two forms: Familial LCAT deficiency, in which there is complete LCAT deficiency, and Fish-eye disease, in which there is a partial deficiency.
Blood lipids are lipids in the blood, either free or bound to other molecules. They are mostly transported in a phospholipid capsule, and the type of protein embedded in this outer shell determines the fate of the particle and its influence on metabolism. Examples of these lipids include cholesterol and triglycerides. The concentration of blood lipids depends on intake and excretion from the intestine, and uptake and secretion from cells. Hyperlipidemia is the presence of elevated or abnormal levels of lipids and/or lipoproteins in the blood, and is a major risk factor for cardiovascular disease.

Evacetrapib was a drug under development by Eli Lilly & Company that inhibits cholesterylester transfer protein. CETP collects triglycerides from very low-density lipoproteins (VLDL) or low-density lipoproteins (LDL) and exchanges them for cholesteryl esters from high-density lipoproteins (HDL), and vice versa, but primarily increasing high-density lipoprotein and lowering low-density lipoprotein. It is thought that modifying lipoprotein levels modifies the risk of cardiovascular disease. The first CETP inhibitor, torcetrapib, was unsuccessful because it increased levels of the hormone aldosterone and increased blood pressure, which led to excess cardiac events when it was studied. Evacetrapib does not have the same effect. When studied in a small clinical trial in people with elevated LDL and low HDL, significant improvements were noted in their lipid profile.
The vertical auto profile (VAP) test is a cholesterol, lipid and lipoprotein test.
Remnant cholesterol, also known as remnant lipoprotein, is a very atherogenic lipoprotein composed primarily of very low-density lipoprotein (VLDL) and intermediate-density lipoprotein (IDL). Stated another way, remnant cholesterol is all plasma cholesterol that is not LDL cholesterol or HDL cholesterol, which are triglyceride-poor lipoproteins. However, remnant cholesterol is primarily chylomicron and VLDL, and each remnant particle contains about 40 times more cholesterol than LDL.